Achalasia is a rare disorder that affects the ability of the esophagus to move food down to the stomach. It is caused by damage to the nerves that control the smooth muscles of the esophagus, resulting in difficulty swallowing, chest pain, and other symptoms. If left untreated, achalasia can lead to serious complications, such as aspiration pneumonia and gastroesophageal reflux disease (GERD). In this article, we will provide an in-depth overview of achalasia, including its symptoms, causes, diagnosis, treatment options, and more.
Understanding Achalasia: Definition and Overview
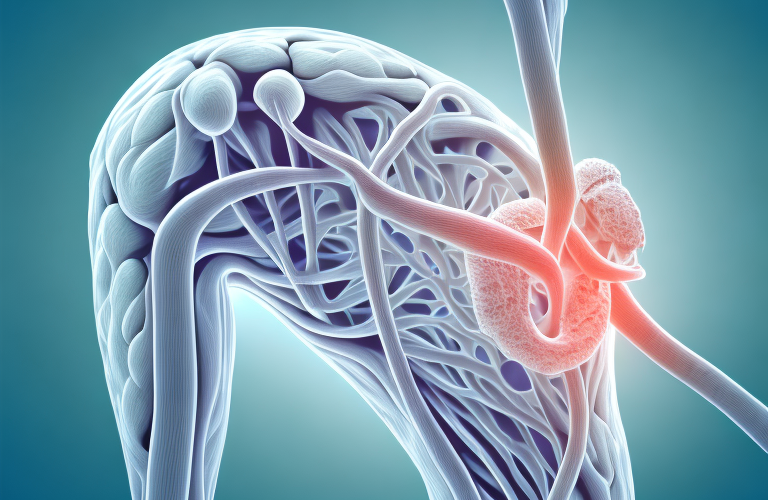
Achalasia is a rare disorder that affects the esophagus, the muscular tube that connects the mouth to the stomach. It is characterized by the inability of the lower esophageal sphincter (LES) to relax, which makes it difficult for food and liquid to pass through the esophagus and into the stomach. The LES is a ring of muscles that acts as a valve, preventing stomach contents from flowing back up into the esophagus. When the LES doesn’t open properly, food and liquid can get trapped in the esophagus, causing discomfort and pain. Achalasia is estimated to affect 1 in every 100,000 people worldwide, and it can occur at any age.
There are several symptoms associated with achalasia, including difficulty swallowing, regurgitation of food, chest pain, and weight loss. These symptoms can be mild or severe, and they can worsen over time if left untreated. In addition to these physical symptoms, achalasia can also have a significant impact on a person’s mental health, causing anxiety and depression due to the challenges of living with a chronic condition.
Treatment for achalasia typically involves a combination of medication, lifestyle changes, and surgical procedures. Medications can help to relax the LES and improve swallowing, while lifestyle changes such as eating smaller meals and avoiding certain foods can also be helpful. In more severe cases, surgery may be necessary to remove or dilate the LES, or to create a new opening in the stomach to allow food to pass through more easily. With proper treatment, most people with achalasia are able to manage their symptoms and maintain a good quality of life.
Symptoms of Achalasia: Difficulty Swallowing, Chest Pain, and More
The most common symptom of achalasia is difficulty swallowing, or dysphagia. This can range from a mild sensation of food getting stuck in the throat to severe blockage that prevents swallowing altogether. Other symptoms may include:
- Chest pain or discomfort
- Regurgitation of food or liquid
- Heartburn or acid reflux
- Unintentional weight loss
- Bloating or abdominal pain
- Coughing or choking while eating or drinking
If you experience any of these symptoms, it is important to seek medical attention as soon as possible.
In addition to the aforementioned symptoms, achalasia can also cause respiratory problems such as pneumonia or bronchitis due to food or liquid entering the lungs. This can lead to coughing, wheezing, and shortness of breath. It is important to note that achalasia is a rare condition and can be difficult to diagnose, so it is crucial to consult with a healthcare professional if you suspect you may have it.
The Causes of Achalasia: Hereditary or Environmental Factors?
The exact cause of achalasia is not yet fully understood. However, it is believed to be caused by a combination of genetic and environmental factors. Some studies have suggested that there may be a genetic link to achalasia, with up to 20% of cases occurring in families with a history of the disorder. Environmental factors, such as viral infections or autoimmune disorders, may also play a role in the development of achalasia. It is important to note that while there are some known risk factors, such as age and gender, achalasia can occur in anyone.
Recent research has also suggested that psychological factors may contribute to the development of achalasia. Stress and anxiety have been linked to the onset of symptoms, and some patients have reported experiencing symptoms after a traumatic event or period of high stress. This highlights the importance of addressing both physical and mental health when treating achalasia.
In addition, certain lifestyle factors may increase the risk of developing achalasia. Obesity, smoking, and a diet high in processed foods have all been associated with an increased risk of the disorder. Making healthy lifestyle choices, such as maintaining a healthy weight and avoiding smoking, may help to reduce the risk of developing achalasia.
Diagnosing Achalasia: Tests and Procedures
Diagnosing achalasia typically involves a combination of medical history, physical examination, and diagnostic tests. Your doctor may first ask about your symptoms and perform a physical exam, which may include checking for signs of reflux, such as heartburn or chest pain. They may also perform an endoscopic evaluation, in which a small, flexible camera is inserted into the esophagus to look for signs of damage or blockage.
Other diagnostic tests that may be used to diagnose achalasia include:
- Esophageal manometry: This test measures the pressure and movement of the muscles in the esophagus and LES.
- Barium swallow: This test involves swallowing a liquid containing barium, which helps to visualize the esophagus and LES on x-rays.
- Endoscopic ultrasound: This test uses ultrasound waves to create a detailed image of the esophagus and surrounding tissues.
If these tests do not provide a clear diagnosis, your doctor may recommend additional tests, such as a CT scan or MRI, to rule out other conditions that may be causing your symptoms. In some cases, a biopsy may also be performed to check for cancer or other abnormalities in the esophagus.
It is important to note that achalasia can be difficult to diagnose, as its symptoms can be similar to those of other conditions, such as gastroesophageal reflux disease (GERD) or esophageal cancer. Therefore, it is important to work closely with your doctor to determine the underlying cause of your symptoms and develop an appropriate treatment plan.
Types of Achalasia: Classic vs. Spastic
There are two main types of achalasia: classic and spastic. Classic achalasia is the most common type and is characterized by a dilated esophagus and incomplete LES relaxation. Spastic achalasia is less common and is characterized by intermittent contractions of the esophagus and LES. Both types of achalasia can cause similar symptoms and complications.
Classic achalasia is typically diagnosed in patients who are middle-aged or older, while spastic achalasia is more commonly diagnosed in younger patients. In addition, classic achalasia is often associated with weight loss and difficulty swallowing solid foods, while spastic achalasia is more commonly associated with chest pain and difficulty swallowing liquids.
Treatment options for both types of achalasia include medications, such as calcium channel blockers and nitrates, as well as minimally invasive procedures like balloon dilation and laparoscopic surgery. However, the best treatment approach will depend on the individual patient’s symptoms, medical history, and overall health.
Complications Associated with Achalasia: Aspiration Pneumonia, GERD, and More
If left untreated, achalasia can lead to serious complications, such as:
- Aspiration pneumonia: This occurs when food or liquid is inhaled into the lungs, causing infection and inflammation.
- GERD: This is a condition in which stomach acid backs up into the esophagus, causing heartburn and other symptoms.
- Esophageal cancer: While rare, long-term untreated achalasia can increase the risk of developing esophageal cancer.
Aside from the aforementioned complications, achalasia can also cause other problems. One of which is weight loss, as patients with achalasia may have difficulty swallowing and may avoid eating altogether. This can lead to malnutrition and other health issues.
Another complication of achalasia is chest pain. Patients may experience chest pain due to the pressure buildup in the esophagus caused by the inability of the muscle to relax and allow food to pass through. This can be mistaken for a heart attack, causing unnecessary anxiety and stress.
Treatment Options for Achalasia: Medications, Surgery, and Lifestyle Changes
Treatment for achalasia typically involves a combination of medications, surgery, and lifestyle changes. The goal of treatment is to relieve symptoms, improve quality of life, and prevent complications.
Medications:
Medications are often used as a first-line therapy for achalasia. These may include:
- Nitrates or calcium channel blockers: These medications help to relax the LES and improve esophageal function.
- Botox injections: This involves injecting botox into the LES, which temporarily paralyzes the muscle and allows food to pass through.
Surgery:
If medications and lifestyle changes are not effective, surgery may be necessary. The most common surgical procedures for achalasia are laparoscopic Heller myotomy and per-oral endoscopic myotomy (POEM). Both procedures involve cutting the muscles of the LES to allow for easier food passage.
Lifestyle Changes:
In addition to medications and surgery, lifestyle changes can help manage symptoms of achalasia. These may include:
- Eating small, frequent meals throughout the day
- Avoiding foods that are difficult to swallow, such as dry or tough meats
- Eating slowly and chewing food thoroughly
- Avoiding carbonated beverages and alcohol
- Elevating the head of the bed at night to prevent reflux
It is important to note that achalasia is a chronic condition and may require ongoing treatment and management. Regular follow-up appointments with a healthcare provider are recommended to monitor symptoms and adjust treatment as needed. In some cases, additional procedures or therapies may be necessary to manage symptoms and prevent complications.
Managing Symptoms of Achalasia: Diet and Nutrition Recommendations
A healthy diet can help manage the symptoms of achalasia and prevent complications. Some dietary recommendations may include:
- Eating small, frequent meals
- Chewing food thoroughly and taking small bites
- Sticking to softer, easy-to-swallow foods
- Drinking plenty of water to aid in digestion
- Avoiding foods and beverages that trigger acid reflux
In addition to dietary changes, there are other lifestyle modifications that can help manage the symptoms of achalasia. These may include:
- Eating meals at least 2-3 hours before bedtime to allow for proper digestion
- Remaining upright for at least 30 minutes after eating to prevent reflux
- Avoiding tight-fitting clothing that can put pressure on the stomach
- Reducing stress through relaxation techniques such as yoga or meditation
If dietary and lifestyle modifications are not effective in managing symptoms, there are medical and surgical treatments available. These may include medications to relax the lower esophageal sphincter, pneumatic dilation to widen the esophagus, or surgery to remove the lower esophageal sphincter. It is important to discuss all treatment options with a healthcare provider to determine the best course of action.
Coping with the Emotional Impact of Living with Achalasia
Achalasia can have a significant emotional impact on those who live with the disorder. It can be frustrating and isolating to deal with the symptoms and limitations of achalasia. It is important to seek support from loved ones, healthcare professionals, and support groups. There are also resources available to help cope with the emotional impact of achalasia, such as counseling or therapy.
One of the most challenging aspects of living with achalasia is the impact it can have on one’s mental health. Many people with achalasia experience anxiety and depression as a result of the disorder. This can be due to the stress of managing symptoms, the fear of choking or aspirating, and the social isolation that can come with difficulty eating in public.
It is important for individuals with achalasia to prioritize their mental health and seek out resources to help manage these emotions. This may include talking to a therapist or counselor, joining a support group, or practicing relaxation techniques such as meditation or yoga. By taking care of their emotional well-being, individuals with achalasia can improve their overall quality of life and better manage the challenges of living with the disorder.
Prognosis for People Living with Achalasia
The prognosis for people living with achalasia is generally good with appropriate treatment. While there is no known cure for achalasia, most people can manage their symptoms and prevent complications with medication, surgery, and lifestyle changes.
However, it is important to note that the success of treatment can vary depending on the severity of the condition and the individual’s response to treatment. In some cases, additional procedures or surgeries may be necessary to achieve symptom relief.
It is also important for individuals with achalasia to maintain regular follow-up appointments with their healthcare provider to monitor their condition and adjust treatment as needed. With proper management, most people with achalasia can lead a normal, healthy life.
Research Developments in the Treatment of Achalasia
Researchers are actively studying new treatments for achalasia, including innovative surgical techniques and alternative therapies. Some studies have suggested that stem cell therapy may be a promising option for restoring nerve function in the esophagus and LES. Other ongoing research focuses on identifying the genetic and environmental factors that contribute to the development of achalasia. By understanding the underlying causes of achalasia, researchers hope to develop targeted treatments that can improve outcomes and quality of life for those with the disorder.
In conclusion, achalasia is a rare disorder that affects the esophagus and can cause difficulty swallowing, chest pain, and other symptoms. While the exact causes of achalasia are not fully understood, there are effective treatments available, such as medications, surgery, and lifestyle changes. It is important to seek prompt medical attention if you experience symptoms of achalasia to prevent complications and ensure the best possible outcomes.
Recent studies have also shown that behavioral therapies, such as biofeedback and relaxation techniques, may be helpful in managing symptoms of achalasia. These therapies aim to reduce stress and anxiety, which can exacerbate symptoms and make it more difficult to swallow. Additionally, dietary changes, such as eating smaller, more frequent meals and avoiding foods that are difficult to swallow, may also be beneficial for those with achalasia.