Barrett’s Esophagus is a medical condition that results in a change in the cells lining the lower part of the esophagus. This is typically caused by prolonged exposure to acid reflux which damages the esophageal lining over time. In this comprehensive guide, we will explore the causes, symptoms, available treatments, and preventative measures for Barrett’s Esophagus.
Understanding Barrett’s Esophagus: A Comprehensive Guide
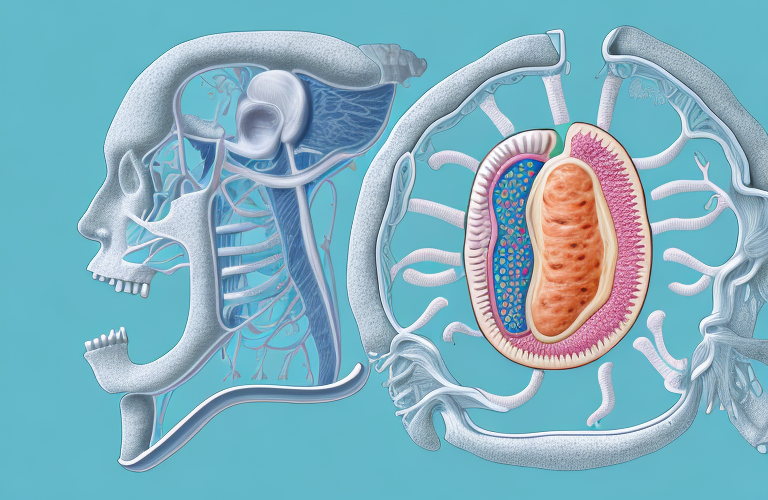
Barrett’s Esophagus is known to cause a change in the cells of the lower esophagus, which makes them more similar to the cells that line the small intestine. While there are no visible symptoms, this change can increase the risk of developing esophageal cancer. Experts believe that acid reflux is the primary cause of this condition, and the change in cells is the body’s way of protecting the esophagus from further damage.
It is estimated that about 10% of people with chronic acid reflux will develop Barrett’s Esophagus. However, not everyone with Barrett’s Esophagus will develop esophageal cancer. Regular monitoring and treatment of acid reflux can help reduce the risk of cancer development.
Treatment options for Barrett’s Esophagus include medication to reduce acid reflux, lifestyle changes such as weight loss and avoiding trigger foods, and in some cases, surgery. It is important to work closely with a healthcare provider to determine the best treatment plan for each individual case.
What is Barrett’s Esophagus and How is it Diagnosed?
Barrett’s Esophagus is a disorder that is diagnosed through procedures like an endoscopy or a biopsy. During an endoscopy, a long, flexible tube is inserted through the mouth into the esophagus and images are taken to observe any changes in the cells. In some cases, a biopsy is done to examine the tissue for any abnormalities and confirm the diagnosis.
Barrett’s Esophagus is a condition where the lining of the esophagus changes and becomes more like the lining of the intestine. This can increase the risk of developing esophageal cancer. It is often associated with chronic acid reflux or gastroesophageal reflux disease (GERD). Treatment options for Barrett’s Esophagus include medication to reduce acid reflux, lifestyle changes, and in some cases, surgery. Regular monitoring through endoscopies and biopsies is also recommended to detect any changes in the cells and prevent the development of cancer.
Who is at Risk of Developing Barrett’s Esophagus?
Barrett’s Esophagus is typically diagnosed in individuals over the age of 50 who have experienced frequent acid reflux symptoms for a prolonged period of time. The risk of developing this condition is higher for individuals who are obese, smoke cigarettes, or have a family history of Barrett’s Esophagus.
Additionally, individuals who have a history of gastroesophageal reflux disease (GERD) or have a weakened immune system may also be at a higher risk of developing Barrett’s Esophagus. It is important to note that while these factors may increase the likelihood of developing the condition, not all individuals with these risk factors will develop Barrett’s Esophagus.
Common Symptoms of Barrett’s Esophagus You Need to Know
Most individuals with Barrett’s Esophagus do not experience any noticeable symptoms. However, some common symptoms include chronic heartburn, difficulty swallowing, chest pain, and hoarseness. These symptoms are typically related to acid reflux, which is one of the common causes of Barrett’s Esophagus.
It is important to note that not all individuals with Barrett’s Esophagus experience symptoms, which is why regular screenings are recommended for individuals who are at a higher risk of developing this condition. Some of the risk factors include being over the age of 50, having a history of acid reflux or GERD, being overweight or obese, and smoking. If left untreated, Barrett’s Esophagus can increase the risk of developing esophageal cancer, which is why early detection and treatment are crucial.
Is Barrett’s Esophagus a Precursor to Cancer?
While Barrett’s Esophagus itself is not cancerous, it can lead to a higher risk of developing esophageal cancer. According to research, individuals with Barrett’s Esophagus have a thirty to one hundred and twenty times higher risk of developing esophageal cancer than those who do not have the condition. It is essential to get regular screenings and seek medical attention immediately if any new symptoms arise.
Studies have shown that the risk of developing esophageal cancer increases with the duration of Barrett’s Esophagus. Individuals who have had the condition for more than ten years are at a higher risk of developing cancer. However, it is important to note that not all cases of Barrett’s Esophagus progress to cancer, and early detection and treatment can significantly improve outcomes.
The Link between Acid Reflux and Barrett’s Esophagus
Acid reflux and Barrett’s Esophagus are deeply connected. Acid reflux is a condition that leads to the damage of the lower esophagus, which can eventually lead to the development of Barrett’s Esophagus. The condition can also aggravate existing Barrett’s Esophagus symptoms, making it essential to seek early diagnosis and effective treatment.
Barrett’s Esophagus is a condition where the lining of the esophagus changes, becoming more like the lining of the intestine. This change in the lining is caused by long-term exposure to stomach acid, which is often the result of chronic acid reflux. If left untreated, Barrett’s Esophagus can increase the risk of developing esophageal cancer. Therefore, it is important to manage acid reflux symptoms and undergo regular screenings to detect any changes in the esophagus early on.
Types of Treatments Available for Barrett’s Esophagus
There are several effective treatments available for Barrett’s Esophagus depending on the severity of the condition. Medications, lifestyle changes, endoscopic treatments, and surgery are all available options. Treatment is typically recommended once the disease starts progressing towards cancer.
Medications such as proton pump inhibitors (PPIs) can help reduce acid reflux and inflammation in the esophagus. Lifestyle changes such as avoiding trigger foods, losing weight, and quitting smoking can also help manage symptoms and prevent further damage. Endoscopic treatments such as radiofrequency ablation (RFA) and cryotherapy can remove abnormal cells and promote healthy tissue growth. In more severe cases, surgery may be necessary to remove the affected tissue. It is important to work with a healthcare provider to determine the best treatment plan for each individual case.
Medications for Managing Symptoms of Barrett’s Esophagus
Most individuals with Barrett’s Esophagus experience symptoms of Acid Reflux. Over-the-counter antacids like Tums, Maalox, and Mylanta can provide temporary symptom relief. Proton-Pump Inhibitors like Nexium, Prevacid, and Prilosec are also available with a prescription and are effective in reducing acid reflux symptoms.
In addition to antacids and proton-pump inhibitors, H2 blockers like Zantac and Pepcid can also be used to manage symptoms of Barrett’s Esophagus. These medications work by reducing the amount of acid produced in the stomach. It is important to consult with a healthcare provider to determine the best medication and dosage for managing symptoms of Barrett’s Esophagus.
Lifestyle Changes to Manage Barrett’s Esophagus
Lifestyle changes can significantly improve the symptoms of Barrett’s Esophagus and reduce the risk of complications. Individuals with the condition should quit smoking, avoid consuming alcohol and caffeine, maintain a healthy weight, and avoid eating large meals or spicy or acidic foods.
In addition to these lifestyle changes, it is also recommended that individuals with Barrett’s Esophagus elevate the head of their bed by 6-8 inches to prevent stomach acid from flowing back into the esophagus while sleeping. It is also important to wait at least 2-3 hours after eating before lying down to allow the stomach to empty properly. Regular exercise and stress management techniques such as yoga or meditation can also help manage symptoms and improve overall health.
Endoscopic Treatment Options for Barrett’s Esophagus
Endoscopic treatments are a non-invasive option for individuals with Barrett’s Esophagus that are not responding to medication and lifestyle changes. Endoscopic therapies like Radiofrequency Ablation (RFA), Endoscopic Mucosal Resection (EMR), and Cryotherapy use specialized equipment to destroy the abnormal cells in the esophagus.
It is important to note that endoscopic treatments are not a cure for Barrett’s Esophagus, but rather a way to manage the condition and prevent it from progressing to esophageal cancer. Regular follow-up appointments with a gastroenterologist are necessary to monitor the effectiveness of the treatment and detect any potential complications.
Surgical Options for Advanced Cases of Barrett’s Esophagus
Surgery is typically recommended for individuals with advanced stages of Barrett’s Esophagus or with a high risk of developing esophageal cancer. The most common surgery is Nissen Fundoplication, where the surgeon wraps the upper part of the stomach around the lower esophageal sphincter to prevent stomach acid from flowing into the esophagus.
Another surgical option for advanced cases of Barrett’s Esophagus is endoscopic mucosal resection (EMR). This procedure involves removing the abnormal tissue lining the esophagus using an endoscope. EMR is less invasive than Nissen Fundoplication and may be a better option for individuals who are not good candidates for traditional surgery.
How to Prevent the Progression of Barrett’s Esophagus
Preventing the progression of Barrett’s Esophagus is critical in reducing the risk of esophageal cancer. Making significant lifestyle changes like quitting smoking, avoiding alcohol, and consuming a healthy diet is the most effective preventative measure. Regular screening tests can also aid in the early detection of abnormal cell changes in the esophagus and prevent the progression of the condition.
In addition to lifestyle changes and regular screening tests, medication can also be prescribed to prevent the progression of Barrett’s Esophagus. Proton pump inhibitors (PPIs) are commonly prescribed to reduce acid reflux and inflammation in the esophagus, which can help prevent the development of abnormal cells. It is important to consult with a healthcare provider to determine the best course of treatment for preventing the progression of Barrett’s Esophagus.
Living with Barrett’s Esophagus: Coping Strategies and Support Groups
Living with Barrett’s Esophagus can be challenging, both physically and emotionally. Developing coping strategies and seeking support from family, friends, and support groups can help manage the emotional stress associated with the condition. Individuals are encouraged to stay informed about their condition, stay regular with treatment plans, and seek professional help when required.
In conclusion, Barrett’s Esophagus is a complex medical condition that requires prompt diagnosis and effective treatment. It is essential for individuals to understand the symptoms, causes, treatments, and preventative measures associated with the condition to improve their quality of life and reduce the risk of complications.
One coping strategy for individuals with Barrett’s Esophagus is to make dietary changes. Avoiding foods that trigger acid reflux, such as spicy or acidic foods, can help reduce symptoms. Eating smaller, more frequent meals and avoiding eating before bedtime can also be helpful. Additionally, quitting smoking and reducing alcohol consumption can improve symptoms and overall health.
Support groups can also be a valuable resource for individuals with Barrett’s Esophagus. These groups provide a safe space for individuals to share their experiences, ask questions, and receive emotional support. Support groups can also provide access to educational resources and information about new treatments and research.