If you experience clitoral pain, you’re certainly not alone. Clitorodynia – or painful clitoris – is a condition that can occur in women of all ages, and it can be an extremely debilitating experience. In this comprehensive article, we will explore the underlying causes of clitoral pain, its common symptoms, diagnostic tests, and various treatment options available to alleviate the discomfort and pain associated with the condition. So, let’s dive right in!
Understanding Clitoral Pain: An Overview
When it comes to evaluating clitoral pain, there’s often a lot of confusion surrounding what it actually is and what can cause it. Essentially, clitorodynia refers to any pain or discomfort that relates to the clitoris. This can include sensations of a burning, stinging, itching, stabbing, or dull aching pain. The intensity can vary greatly from mild to severe, with the pain often being exacerbated by touch, pressure, or sexual activity.
There are several potential causes of clitoral pain, including infections, nerve damage, hormonal imbalances, and certain medical conditions such as endometriosis or vulvodynia. It’s important to seek medical attention if you experience persistent or severe clitoral pain, as it could be a sign of a more serious underlying issue.
Treatment for clitoral pain will depend on the underlying cause, but may include medications, physical therapy, or lifestyle changes. It’s also important to communicate openly with your healthcare provider and sexual partner(s) about any pain or discomfort you may be experiencing, as this can help ensure that you receive the appropriate care and support.
Types of Clitoral Pain: Explained
Clitoral pain can present in various ways, depending on its underlying cause. Some women may experience pain only during sexual intercourse, while others may feel discomfort throughout the day, even when engaging in non-sexual activities. Moreover, some women may experience pain near the clitoris, while others might feel it deep inside the pelvic area. The following is a brief overview of the various types of clitoral pain:
- Vulvar pain – Located around the opening of the vagina and vulva, this can cause burning or shooting pain in the clitoral region.
- Vestibulodynia – Pain in the vestibule area of the vulva, which surrounds the vagina.
- Clitoral hypersensitivity – Sensitivity or discomfort caused by over-stimulation of the clitoris.
- Clitoral phimosis – A condition where the clitoral hood can’t be retracted easily or at all, causing discomfort and occasionally pain.
It is important to note that clitoral pain can also be a symptom of an underlying medical condition, such as endometriosis or pelvic inflammatory disease. In these cases, the pain may be accompanied by other symptoms, such as heavy menstrual bleeding or fever. It is important to seek medical attention if you experience persistent or severe clitoral pain, especially if it is affecting your daily life or sexual function.
What Causes Clitoral Pain and Discomfort?
There are numerous possible causes of clitoral pain, ranging from medical conditions to psychological triggers:
- Infections, such as a yeast infection or bacterial vaginosis, can cause vulvar pain and even clitoral pain.
- Sexually transmitted infections (STIs) such as genital herpes, gonorrhea, or chlamydia can also cause significant discomfort.
- Vulvodynia – A chronic pain condition that affects the vulva and can lead to increased sensitivity in the clitoral region.
- Vulvar cancer or other benign tumors can cause pain and discomfort around the clitoris.
- Damage to the pelvic area or nerves connecting to the clitoris can cause clitoral pain.
- Poor hygiene, harsh detergents or soaps, or tight clothing can lead to clitoral irritation.
- Psychological causes such as anxiety, depression, or a history of sexual abuse can also cause painful sensations around the clitoris.
It is important to note that clitoral pain and discomfort can also be caused by certain medications, such as antidepressants or blood pressure medications. These medications can affect the nerve endings in the clitoral region, leading to pain or numbness. If you are experiencing clitoral pain or discomfort, it is important to speak with your healthcare provider to determine the underlying cause and receive appropriate treatment.
Common Symptoms of Clitorodynia You Should Know
The most noticeable symptom of clitorodynia is pain in or around the clitoris. It can be a general pain or specific to certain positions or activities. Other common symptoms include:
- Burning or stinging sensations around the clitoris
- Itching or tingling sensations
- Tenderness or soreness in the clitoral region
- Difficulty achieving orgasm
- Pain during sex or difficulty with penetration
- Increased sensitivity in the clitoral area
Clitorodynia is a condition that affects many women and can have a significant impact on their quality of life. It is important to note that the severity of symptoms can vary from person to person, and some women may experience more severe symptoms than others.
In addition to the physical symptoms, clitorodynia can also have emotional and psychological effects. Women with this condition may experience anxiety, depression, and a decreased interest in sexual activity. It is important for women to seek medical attention if they are experiencing any of these symptoms, as there are treatments available that can help alleviate the pain and discomfort associated with clitorodynia.
Medical Conditions That Can Lead to Clitoral Pain
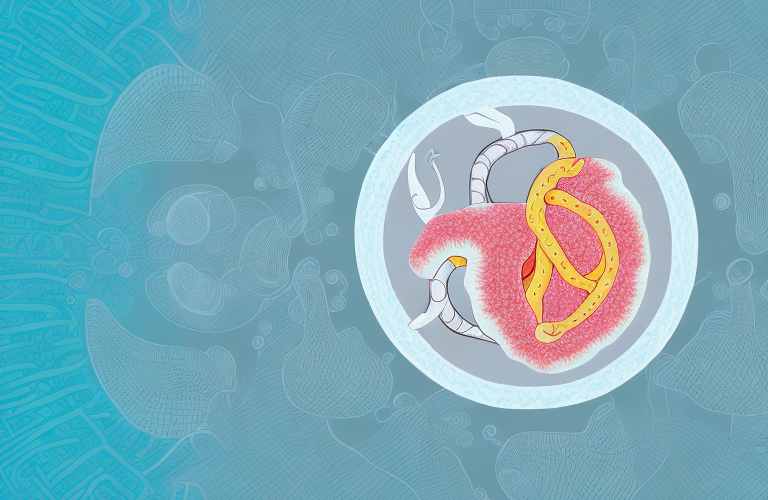
Various medical conditions can cause clitoral pain. For instance, vulvodynia is a condition that causes chronic pain in the vulvar area, which can spread to the clitoris. Other medical conditions that can lead to clitoral pain include:
- Endometriosis: A condition wherein endometrial tissue grows outside the uterus
- Vaginitis: Inflammation of the vagina
- Vulvar cancer or other benign tumors
- Interstitial cystitis: A condition that causes bladder pain and pelvic pain
Another medical condition that can cause clitoral pain is pelvic inflammatory disease (PID). PID is an infection of the female reproductive organs, which can cause pain in the clitoris, as well as other areas of the pelvic region.
Additionally, clitoral pain can also be a side effect of certain medications, such as antidepressants and antihistamines. If you are experiencing clitoral pain, it is important to speak with your healthcare provider to determine the underlying cause and receive appropriate treatment.
Psychological Causes of Clitoral Pain and How to Manage Them
Psychological factors such as anxiety, depression, and a history of sexual abuse or trauma can lead to clitoral pain. These can be challenging to diagnose, but when identified, a combination of talk therapy, lifestyle changes, and medication can be used.
It is important to note that clitoral pain can also be a symptom of other psychological conditions such as somatic symptom disorder or vulvodynia. These conditions require a thorough evaluation by a healthcare professional to determine the underlying cause and appropriate treatment plan.
In addition to talk therapy and medication, lifestyle changes such as stress reduction techniques, regular exercise, and a healthy diet can also help manage clitoral pain caused by psychological factors. It is important to work with a healthcare provider to develop a comprehensive treatment plan that addresses both the physical and psychological aspects of clitoral pain.
Diagnosing Clitoral Pain: Tests and Examinations Involved
The diagnosis of clitoral pain often requires a thorough physical examination and a series of accompanying tests. Typically, this might involve:
- A pelvic exam to determine whether there are any visible signs of irritation or infection.
- Laboratory tests to rule out STIs, candida infections, or other bacterial infections;
- Biopsy to diagnose the possibility of vulvar cancer or other tumors
- Urine tests, MRI, or CT scan to rule out the possibility of interstitial cystitis or other bladder conditions
In addition to the above-mentioned tests, doctors may also perform a sensory exam to determine the extent of nerve damage or sensitivity in the clitoral area. This may involve using a cotton swab or other instrument to test the patient’s response to touch or pressure.
It is also important for doctors to take a detailed medical history of the patient, including any medications they are currently taking, as certain medications can cause clitoral pain as a side effect. Additionally, doctors may ask about the patient’s sexual history and practices, as certain sexual activities or positions can also contribute to clitoral pain.
Treatment Options for Clitorodynia: Medications, Therapies, and Procedures
Clitorodynia treatment aims to alleviate the associated pain and discomfort. Here are the available options:
- Pain medications such as lidocaine or gabapentin
- Hormonal replacement therapy for menopausal women
- Ultrasound therapy to help damaged tissues heal
- Biofeedback to try to reduce sensitivity to clitoral stimulation
- Topical estrogen treatment to reduce pain
- Nerve blocks to provide localized anesthetic
- Cognitive-behavioral therapy or sex counseling to help with psychological causes
- Surgery to remove a benign tumor or damaged tissue to relieve discomfort or pain
It is important to note that the effectiveness of these treatments may vary depending on the underlying cause of clitorodynia. In some cases, a combination of treatments may be necessary to achieve relief. It is recommended to consult with a healthcare provider to determine the best course of action for individual cases.
Lifestyle Changes That Can Help Alleviate Clitoral Pain
Self-care measures can be helpful in reducing symptoms of clitoral pain:
- Wearing comfortable clothing made with breathable fabric and avoiding tight-fitting pants and underwear
- Using mild and fragrance-free soaps and detergents for washing
- Practicing relaxation techniques such as yoga or meditation
- Using a cool compress to soothe pain and irritation
- Avoiding sexual intercourse or using condoms to reduce the risk of infections
Aside from the self-care measures mentioned above, there are other lifestyle changes that can help alleviate clitoral pain. One of these is maintaining a healthy diet and staying hydrated. Eating a balanced diet and drinking plenty of water can help reduce inflammation and promote healing.
Another lifestyle change that can help alleviate clitoral pain is getting enough rest and sleep. Lack of sleep can weaken the immune system and increase inflammation, which can worsen pain and discomfort. Getting enough rest and sleep can help the body heal and reduce symptoms of clitoral pain.
Coping with Chronic Clitoral Pain: Tips and Strategies to Try
Living with chronic clitoral pain can be challenging, but adopting certain strategies can help alleviate the discomfort. Here are some tips you can try:
- Practice mindfulness meditation to focus your attention on the present moment and relieve anxiety or stress levels
- Join a support group to find resources, helpful tips, and emotional support from other women who experience clitoral pain
- Stay physically active, as exercise can improve your overall physical and emotional health, and reduce pain levels
- Consider alternative pain management techniques such as acupuncture, massage therapy, or hypnosis to help manage your symptoms
It is important to note that chronic clitoral pain can have a significant impact on a person’s mental health. It can lead to feelings of isolation, depression, and anxiety. Seeking professional help from a therapist or counselor can be beneficial in managing these emotions and improving overall well-being.
In addition, it is important to communicate openly with your partner about your pain and how it may affect sexual activity. Exploring alternative forms of intimacy and pleasure, such as non-penetrative sex or using sex toys, can help maintain a fulfilling sexual relationship while managing pain.
Prevention Tips to Avoid Recurring Episodes of Clitorodynia
Preventing clitoral pain typically involves a few key steps:
- Practice good hygiene, including cleaning the clitoral region daily and changing sanitary pads often
- If you are experiencing vaginal dryness, consider using a water-based lubricant during sexual activity
- Avoiding irritants such as tight clothing or harsh soaps
- Using cotton-based underwear instead of synthetic fabrics to reduce irritation and promote hygiene
In addition to the above prevention tips, it is important to communicate with your sexual partner about any discomfort or pain during sexual activity. This can help to avoid further irritation or injury to the clitoral region. It is also recommended to schedule regular check-ups with your healthcare provider to ensure any underlying medical conditions are properly managed.
How to Discuss Your Clitoral Pain with Your Healthcare Provider
If you’re experiencing clitoral pain, it’s essential to talk to your doctor about your symptoms and how they’re affecting your life. Here are some tips to help you start the conversation:
- Make a list of the symptoms you’ve been experiencing, as well as any triggers that may be causing or exacerbating the pain
- Explain your pain level and how it’s affecting your ability to engage in daily activities and sexual activity
- Ask your doctor about the various diagnostic tests available and inquire about the treatment options that may best work for you
- Express any concerns or fears openly to discuss your feelings openly with your doctor
It’s important to note that clitoral pain can be caused by a variety of factors, including infections, nerve damage, and hormonal imbalances. Your doctor may ask you questions about your medical history, sexual history, and any medications you’re currently taking to help determine the underlying cause of your pain.
Additionally, your doctor may recommend lifestyle changes, such as avoiding tight clothing or using lubrication during sexual activity, to help alleviate your symptoms. In some cases, medication or surgery may be necessary to treat the underlying condition causing your clitoral pain.
Natural Remedies for Clitoral Pain Relief
While some natural remedies may help alleviate clitoral pain, it’s always important to talk to your doctor before trying any new remedies:
- Warm Epsom salt baths to soothe and relax irritated muscles and tissues
- Essential oils like tea tree oil, lavender, or chamomile – diluted with a carrier oil – can have therapeutic effects on reducing inflammation and pain
- Vitamin E supplements, as they promote healthy skin and tissue and may also offer some anti-inflammatory effect
- Acupuncture or acupressure might help alleviate nerve pain associated with clitoral pain but speak to your doctor for a referral to a qualified practitioner
Overall, clitoral pain can be a complex condition, but with the right diagnosis and treatment plan, it can be managed effectively. Don’t hesitate to reach out to your doctor for help if you’re experiencing persistent clitoral pain.
In addition to the natural remedies mentioned above, there are other lifestyle changes that may help alleviate clitoral pain. For example, avoiding tight clothing and underwear can reduce irritation and pressure on the clitoris. Additionally, practicing relaxation techniques such as yoga or meditation can help reduce stress and tension in the pelvic area, which may contribute to clitoral pain.
It’s also important to note that clitoral pain can sometimes be a symptom of an underlying medical condition, such as vulvodynia or endometriosis. If you’re experiencing persistent or severe clitoral pain, it’s important to speak with your doctor to rule out any underlying conditions and determine the best course of treatment.