The topic of genitals is often considered taboo, but it is important to understand how these organs function and why they are essential for reproduction and sexual pleasure. In this comprehensive guide, we will explore the vital role of genital anatomy and function while debunking common misconceptions about these organs.
The Importance of Understanding Genital Anatomy
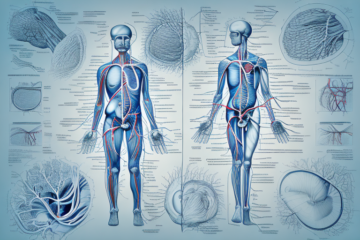
Before delving into the specifics of male and female genital anatomy, it is essential to understand their general structure. The genitals are located in the pelvic area and include a variety of organs, such as the penis, scrotum, testes, ovaries, vagina, and clitoris. Each of these organs has a unique function that plays a crucial role in human reproduction and sexual pleasure.
One important aspect of understanding genital anatomy is recognizing the differences between male and female genitalia. While both sexes have similar structures, such as the clitoris and penis, there are also distinct differences in size, shape, and function. Understanding these differences can help individuals better understand their own bodies and those of their partners.
Another important consideration is the role that hormones play in genital development and function. Hormones such as testosterone and estrogen have a significant impact on the development and maintenance of male and female genitalia, as well as sexual desire and function. Understanding the role of hormones in sexual health can help individuals make informed decisions about their own bodies and seek appropriate medical care when necessary.
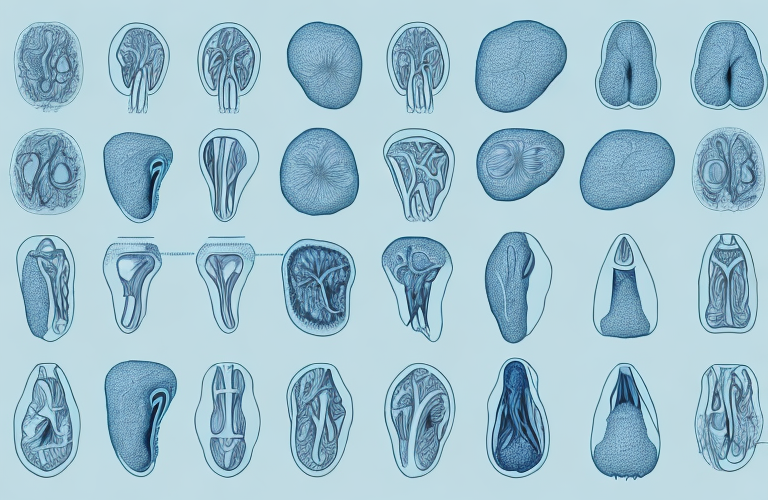
Male Genital Anatomy: An In-Depth Look
The male genital anatomy comprises several organs, including the penis, testicles, scrotum, and prostate gland. The penis is the primary male sexual organ responsible for intercourse and urination. The testicles are responsible for producing testosterone, the male sex hormone, and sperm. The scrotum houses the testicles and keeps them at a temperature lower than the body’s core temperature. Lastly, the prostate gland is responsible for producing seminal fluid, which is a vital component of semen.
It is important to note that the male genital anatomy can vary in size, shape, and color. The size of the penis can range from a few inches to over a foot in length when erect. The color of the penis and scrotum can also vary, with some individuals having darker or lighter skin tones. Additionally, some men may have a condition called hypospadias, where the opening of the urethra is located on the underside of the penis instead of at the tip. Understanding the variations in male genital anatomy can help individuals better understand their own bodies and promote body positivity.
Female Genital Anatomy: The Complexities Explored
The female genital anatomy is more complex than its male counterpart and includes the vagina, cervix, uterus, fallopian tubes, clitoris, labia, and ovaries. The vagina is a muscular tubular organ that connects the uterus to the outside body, and it serves as the primary organ for sexual intercourse, menstruation, and childbirth. The cervix is the lower portion of the uterus that connects to the vagina, while the uterus is responsible for carrying a developing fetus. The ovaries produce and release eggs while also releasing hormones essential for female reproductive cycles.
The clitoris is a highly sensitive organ located at the front of the vulva, and it plays a crucial role in female sexual pleasure. The labia, which are the outer and inner folds of skin surrounding the vaginal opening, protect the genital area and also contain nerve endings that contribute to sexual sensation. The fallopian tubes are two thin tubes that extend from the uterus to the ovaries, and they are responsible for transporting eggs from the ovaries to the uterus. Understanding the complexities of female genital anatomy is essential for maintaining reproductive health and sexual well-being.
The Role of Hormones in Genital Development
Hormones play a vital role in genital development, influencing everything from genital size and shape to sexual orientation and desire. The two primary hormones that regulate genital development and function are testosterone and estrogen. Testosterone is essential for the development of male genitalia, while estrogen plays a crucial role in the development of female genitalia.
However, it is important to note that hormones can also play a role in intersex conditions, where an individual’s genitalia do not fit typical male or female classifications. In some cases, hormonal imbalances during fetal development can lead to ambiguous genitalia or the development of both male and female genitalia.
Furthermore, hormones continue to play a role in genital function throughout an individual’s life. Testosterone, for example, is responsible for maintaining male sexual function and libido, while estrogen helps to regulate the menstrual cycle and vaginal health in females. Hormonal imbalances in adulthood can lead to a range of issues, including infertility, sexual dysfunction, and even certain types of cancer.
A Comprehensive Guide to Genital Function
The primary function of the genitals is to facilitate sexual pleasure and reproduction. During sexual arousal, the genitals become engorged with blood, leading to an increase in sensitivity and pleasure. In males, this arousal leads to an erection and the eventual ejaculation of semen. Females experience vaginal lubrication and swelling during arousal, and many experience orgasm as a result of clitoral stimulation.
However, the function of the genitals goes beyond sexual pleasure and reproduction. In males, the testes produce testosterone, which is responsible for the development of male secondary sexual characteristics such as facial hair, deepening of the voice, and muscle growth. In females, the ovaries produce estrogen and progesterone, which regulate the menstrual cycle and are responsible for the development of female secondary sexual characteristics such as breast growth and widening of the hips.
Additionally, the genitals play a role in urinary function. The urethra, which is a tube that carries urine from the bladder to the outside of the body, passes through the penis in males and is located near the vaginal opening in females. The muscles of the pelvic floor, which support the bladder and bowel, are also located in the genital area.
What Happens During Sexual Arousal?
Sexual arousal leads to a range of physiological responses in the body, including increased heart rate, blood pressure, and respiration. Hormones like testosterone and estrogen also play a role in arousal, leading to an increase in sexual desire and sensation. The genitals also become engorged with blood, leading to an increase in sensitivity and pleasure.
Additionally, sexual arousal can also lead to changes in the body’s musculature, including increased muscle tension and contractions. These muscle contractions can contribute to the pleasurable sensations experienced during sexual activity, and can also help facilitate orgasm.
Furthermore, sexual arousal can also have psychological effects, such as increased feelings of intimacy and emotional connection with a partner. This can be attributed to the release of hormones like oxytocin, which is often referred to as the “love hormone” due to its role in promoting bonding and attachment.
The Mechanics of Erection and Ejaculation in Males
Erection and ejaculation are essential components of male sexual function. An erection occurs when the penis becomes engorged with blood, leading to an increase in size and sensitivity. Ejaculation occurs when semen is expelled from the penis during orgasm, leading to a feeling of intense pleasure. These processes are governed by a complex interplay of hormones, nerves, and blood vessels.
During an erection, the penis is filled with blood due to the relaxation of smooth muscles in the blood vessels. This relaxation is triggered by the release of nitric oxide, a chemical messenger that signals the blood vessels to dilate. The increased blood flow to the penis causes it to become rigid and erect. However, the process of achieving and maintaining an erection can be affected by various factors such as stress, anxiety, and certain medical conditions.
Ejaculation, on the other hand, is a reflex action that is triggered by the stimulation of nerves in the penis. These nerves send signals to the spinal cord, which in turn sends signals to the muscles in the pelvic area to contract and expel semen from the penis. The amount of semen and the force of ejaculation can vary from person to person and can be affected by factors such as age, frequency of sexual activity, and overall health.
Female Sexual Response: From Arousal to Orgasm
The female sexual response is more complex than his male counterpart and includes several stages. During the arousal phase, the genitals become engorged with blood, leading to an increase in sensitivity and pleasure. During the plateau phase, arousal continues to increase, leading to the eventual orgasmic climax. Lastly, during the resolution phase, the body returns to its pre-arousal state.
It is important to note that not all women experience the same sexual response. Some women may have difficulty reaching orgasm, while others may experience multiple orgasms. Additionally, factors such as stress, medication, and hormonal changes can affect a woman’s sexual response.
Communication with a partner and exploring one’s own body can be helpful in understanding and enhancing the female sexual response. Experimenting with different types of stimulation, such as clitoral or vaginal, can also lead to a more fulfilling sexual experience.
Common Genital Conditions and Disorders
There are numerous conditions and disorders that can affect genital health, ranging from benign to severe. Some common conditions include erectile dysfunction, urinary tract infections, and genital herpes. These conditions can often be treated effectively with medications and lifestyle changes, but it is crucial to seek medical attention as early as possible.
Another common genital condition is bacterial vaginosis, which is caused by an imbalance of bacteria in the vagina. Symptoms include itching, burning, and a strong fishy odor. Treatment typically involves antibiotics and maintaining good hygiene practices.
Additionally, sexually transmitted infections (STIs) such as chlamydia, gonorrhea, and syphilis can also affect genital health. These infections can often be asymptomatic, meaning that individuals may not even know they are infected. It is important to get tested regularly and practice safe sex to prevent the spread of STIs.
Sexually Transmitted Infections: Symptoms, Treatment, and Prevention Strategies
Sexually transmitted infections (STIs) are a significant concern for individuals engaging in sexual behavior. Symptoms of STIs can vary widely and include painful urination, discharge, and sores on the genitals. Treatment for STIs typically involves medication, but prevention strategies like condom use and regular testing are also essential for maintaining genital health.
It is important to note that some STIs may not present with any symptoms at all, making regular testing even more crucial. Additionally, certain STIs can have long-term health consequences if left untreated, such as infertility or an increased risk of certain cancers.
Prevention strategies for STIs also include open communication with sexual partners about sexual health and history, as well as limiting the number of sexual partners. It is also important to note that while condoms can greatly reduce the risk of contracting an STI, they are not 100% effective and do not protect against all types of STIs.
Pregnancy and Childbirth: How the Genitals are Impacted
The genitals are profoundly impacted by pregnancy and childbirth. During pregnancy, the uterus expands to accommodate the developing fetus, leading to changes in the vagina and cervix. Childbirth can cause trauma to the vaginal and perineal tissues, leading to pain and discomfort. Seeking proper medical care during and after pregnancy is essential for maintaining genital health.
It is important to note that the impact of pregnancy and childbirth on the genitals can vary from person to person. Factors such as the size of the baby, the length of labor, and the use of medical interventions can all play a role in the extent of genital trauma. Additionally, hormonal changes during pregnancy and postpartum can also affect genital health. It is recommended that individuals discuss any concerns or symptoms with their healthcare provider to ensure proper care and treatment.
Age-Related Changes in Genital Health and Functioning
The genitals, like the rest of the human body, undergo changes as we age. In both males and females, hormonal changes can lead to a decrease in sexual desire and response. Additionally, men may experience erectile dysfunction due to reduced blood flow to the penis, and women may experience vaginal dryness and pain during intercourse.
However, it is important to note that these changes are not inevitable and can be managed with proper care and attention. Regular exercise, a healthy diet, and avoiding smoking and excessive alcohol consumption can help maintain sexual health and functioning in older adults.
Furthermore, older adults may also face unique challenges in maintaining sexual health, such as the increased risk of sexually transmitted infections (STIs) due to weakened immune systems. It is important for older adults to practice safe sex and get regular STI screenings to prevent and treat any infections.
Maintaining Optimal Genital Health: Tips and Strategies
Maintaining optimal genital health is essential for overall health and wellbeing. Some tips and strategies for maintaining healthy genitals include practicing safe sex, regularly engaging in sexual activity, maintaining a healthy weight, and wearing breathable clothing. It is also essential to get regular checks up to ensure the early detection of any conditions or disorders.
In addition to the above tips, it is important to maintain good hygiene practices to prevent infections and other issues. This includes washing the genital area with mild soap and water, avoiding harsh chemicals or perfumes, and drying the area thoroughly after bathing or swimming. It is also recommended to avoid using douches or other products that can disrupt the natural balance of bacteria in the genital area.
Beyond Binary: Understanding Non-Binary Genitals
While much of the focus of this article has been on male and female genital anatomy, it is essential to recognize that not all individuals fit neatly into these binary categories. Non-binary individuals may have a diverse range of genital configurations, and it is essential to respect and understand these differences.
Non-binary individuals may identify as genderqueer, genderfluid, or agender, and their genital anatomy may not align with traditional male or female characteristics. Some non-binary individuals may have a combination of both male and female genitalia, while others may have genitalia that is not easily categorized as either male or female.
It is important to remember that genital anatomy does not determine an individual’s gender identity, and that everyone’s experience with their own body is unique. By educating ourselves and respecting the diversity of human experience, we can create a more inclusive and accepting society for all individuals, regardless of their gender identity or genital configuration.
The Future of Genital Health Research and Innovations
As our understanding of the genitals continues to evolve, so too will our ability to develop innovative treatments and preventive strategies. Research into genetic and hormonal influences on genital development may lead to new therapies for a range of conditions and disorders. Additionally, developments in robotic and telemedicine technology could revolutionize the way that genital healthcare is delivered.
In conclusion, understanding genital anatomy and function is essential for personal health and wellbeing. By dispelling misconceptions and exploring the complexities of genital health, we can empower individuals to make informed decisions about their sexual and reproductive health.
One area of research that shows promise is the study of the microbiome of the genitals. The microbiome is the collection of microorganisms that live in and on our bodies, and research has shown that imbalances in the genital microbiome can lead to a range of health issues. By better understanding the role of the microbiome in genital health, researchers may be able to develop new treatments and preventive measures.
Another area of innovation in genital healthcare is the development of non-invasive diagnostic tools. Currently, many genital health conditions require invasive procedures for diagnosis, which can be uncomfortable and embarrassing for patients. However, new technologies such as imaging and biomarker testing may allow for more accurate and less invasive diagnosis of genital conditions.