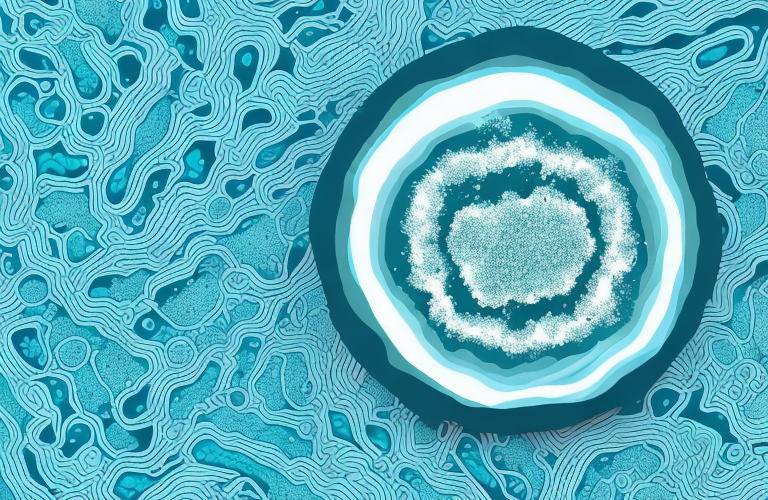
Pseudomonas aeruginosa or P. aeruginosa is a type of bacterium that often causes infections in different parts of the body. It is commonly found in moist environments like soil and water, which makes it an opportunistic pathogen that can easily infect humans when they come into contact with contaminated water, surfaces, or objects.
What is P. aeruginosa and how does it spread?
P. aeruginosa is a type of gram-negative bacterium that has a natural resistance to many antibiotics. It is a common cause of healthcare-associated infections, especially in individuals with weakened immune systems, those who have undergone surgery, or those who require invasive medical devices like catheters or ventilators.
The bacteria can spread through contact with infected surfaces, contaminated water, or exposure to bodily fluids from infected individuals. They can also be spread through direct contact with infected wounds or skin lesions.
It is important to note that P. aeruginosa can also be found in the environment, such as in soil and water. In some cases, individuals may become infected through exposure to contaminated soil or water sources. Additionally, P. aeruginosa can be spread through person-to-person contact, particularly in settings where hygiene practices are not strictly followed, such as in prisons or military barracks.
Symptoms of P. aeruginosa infection
The symptoms of P. aeruginosa infection may vary depending on the location and severity of the infection. Common symptoms of P. aeruginosa infection include:
- Fever
- Chills
- Fatigue
- Cough
- Shortness of breath
- Muscle aches
- Skin rash
- Diarrhea
- Urinary tract infection
- Bloodstream infections
It is important to note that some individuals may not experience any symptoms of P. aeruginosa infection, especially those with weakened immune systems. Additionally, P. aeruginosa infections can be particularly dangerous for individuals with cystic fibrosis, as the bacteria can cause severe lung damage and respiratory failure.
Who is most at risk of developing a P. aeruginosa infection?
Individuals with weakened immune systems due to illness, medical treatment or surgery, and individuals who frequently come into contact with healthcare settings are at increased risk of developing an infection with P. aeruginosa.
Individuals with chronic diseases like cystic fibrosis are also at higher risk of infection due to the bacterium’s ability to colonize and cause the chronic lung infections that are a hallmark of the disease.
Additionally, individuals who use hot tubs or swimming pools that are not properly maintained may also be at risk of developing a P. aeruginosa infection. The bacterium can survive in warm, moist environments and can easily spread in these settings if proper disinfection and cleaning protocols are not followed.
Diagnosing P. aeruginosa: Tests and procedures
A variety of tests and procedures can be used to diagnose P. aeruginosa infection, including:
- Blood tests
- Urine tests
- Imaging scans like X-rays, MRIs or CT scans
- Sputum culture
- Wound culture
In certain cases, a tissue biopsy or bronchoscopy may be necessary to obtain a sample for testing.
It is important to note that P. aeruginosa infections can be difficult to diagnose, as they often present with symptoms similar to other types of infections. Additionally, some strains of P. aeruginosa have developed resistance to certain antibiotics, making treatment more challenging.
Further testing may be necessary to determine the specific strain of P. aeruginosa causing the infection, as well as its antibiotic susceptibility. This can involve genetic testing or susceptibility testing, which can help guide treatment decisions and improve outcomes for patients.
Treatment options for P. aeruginosa infections
Treatment for P. aeruginosa infections may vary depending on the location and severity of the infection. Treatment options may include:
- Antibiotics
- Surgery to remove infected tissue or device
- Supportive care to manage symptoms
It is worth noting that P. aeruginosa is a naturally antibiotic-resistant bacterium, which can make it challenging to treat when it infects severely ill individuals. In some cases, combination therapy or IV antibiotics may be required to manage the infection.
Additionally, prevention measures can also be taken to reduce the risk of P. aeruginosa infections. These measures may include proper hand hygiene, disinfection of medical equipment, and avoiding exposure to contaminated water sources. It is important to follow these prevention measures, especially for individuals with weakened immune systems or those who are hospitalized, as they are at a higher risk of developing P. aeruginosa infections.
Antibiotic resistance in P. aeruginosa: Causes and implications
The natural antibiotic resistance of P. aeruginosa has been exacerbated by the overuse and misuse of antibiotics, which has led to the emergence of antibiotic-resistant strains of the bacterium. This can be problematic for individuals with weakened immune systems who require accurate and effective antimicrobial therapy to manage their infections.
The emergence of multidrug-resistant strains of P. aeruginosa has become a significant public health concern and highlights the critical need for alternative therapeutic approaches that target the bacterium’s virulence factors.
One potential alternative approach is the use of bacteriophages, which are viruses that specifically target and infect bacteria. Bacteriophages have shown promise in treating P. aeruginosa infections, as they can effectively kill the bacterium without harming the body’s natural microbiome. However, further research is needed to fully understand the safety and efficacy of this approach.
Preventing P. aeruginosa infections: Tips for staying healthy
To prevent P. aeruginosa infections, some steps you can take include:
- Washing your hands regularly with soap and water
- Avoiding contact with contaminated surfaces or water
- Keeping their skin clean and dry.
- Proper care and maintenance of medical devices like catheters or ventilators to prevent infection.
Additionally, it is important to avoid close contact with individuals who have P. aeruginosa infections, especially if you have a weakened immune system. It is also recommended to avoid sharing personal items such as towels, razors, or toothbrushes to prevent the spread of the bacteria.
In some cases, antibiotics may be prescribed to prevent or treat P. aeruginosa infections. However, it is important to use antibiotics only as directed by a healthcare professional and to complete the full course of treatment to prevent antibiotic resistance.
The link between P. aeruginosa and cystic fibrosis
Cystic fibrosis is a genetic condition that causes the secretion of thick, sticky mucus in various organs, including the lungs. This creates an ideal environment for the growth and colonization of P. aeruginosa, leading to chronic lung infections that can cause severe lung damage over time.
Treatment for individuals with cystic fibrosis may include antimicrobial therapy, airway clearance techniques, and other supportive measures to manage the symptoms and minimize further organ damage.
Research has shown that P. aeruginosa can adapt and evolve within the lungs of individuals with cystic fibrosis, becoming more resistant to antimicrobial therapy over time. This highlights the importance of early and aggressive treatment to prevent the development of chronic infections and reduce the risk of further lung damage.
Complications of P. aeruginosa infections: What you need to know
If left untreated, P. aeruginosa infections can cause severe complications, including:
- Septicemia
- Endocarditis
- Pneumonia
- Sepsis
- Organ failure
In individuals with chronic lung infections caused by P. aeruginosa, the associated lung damage and inflammation can lead to the development of bronchiectasis, a condition characterized by persistent coughing, shortness of breath, and lung scarring.
Additionally, P. aeruginosa infections can also lead to skin and soft tissue infections, particularly in individuals with weakened immune systems or those who have suffered burns or other skin injuries. These infections can be difficult to treat and may require surgical intervention.
It is important to note that P. aeruginosa is often resistant to multiple antibiotics, making treatment challenging. In some cases, combination therapy with multiple antibiotics may be necessary to effectively treat the infection and prevent complications.
Research updates on P. aeruginosa: Latest discoveries and breakthroughs
Significant progress has been made in recent years regarding the development of new treatment strategies to combat P. aeruginosa infection. Researchers are exploring the potential of novel antibiotics, immunotherapies and phage therapy to target the bacterium’s drug resistance mechanisms and reduce the risk of chronic infections.
Recent studies have also shown that P. aeruginosa can form biofilms, which can make it more difficult to treat and eradicate. Researchers are now investigating ways to disrupt these biofilms, such as using enzymes or other compounds that can break down the extracellular matrix that holds the biofilm together. This could potentially lead to more effective treatments for P. aeruginosa infections and improve patient outcomes.
Living with a chronic P. aeruginosa infection: Coping strategies and support resources
Individuals with chronic P. aeruginosa infections may experience significant challenges managing their symptoms and maintaining their quality of life. They may benefit from support resources like chronic disease management programs, counseling services, and online support groups that can provide information, guidance, and social support.
It is important for individuals with chronic P. aeruginosa infections to work closely with their healthcare providers to manage their symptoms, prevent complications and improve their overall health and well-being.
In conclusion, P. aeruginosa infections can pose significant health risks for individuals with weakened immune systems, chronic diseases, and those who frequently come into contact with healthcare settings. However, with proper prevention and management strategies, as well as ongoing research efforts, it is possible to effectively manage and treat these infections and improve outcomes for those affected.
One important coping strategy for individuals with chronic P. aeruginosa infections is to maintain a healthy lifestyle. This includes eating a balanced diet, getting regular exercise, and getting enough sleep. These lifestyle factors can help boost the immune system and improve overall health, which can in turn help manage symptoms and prevent complications.