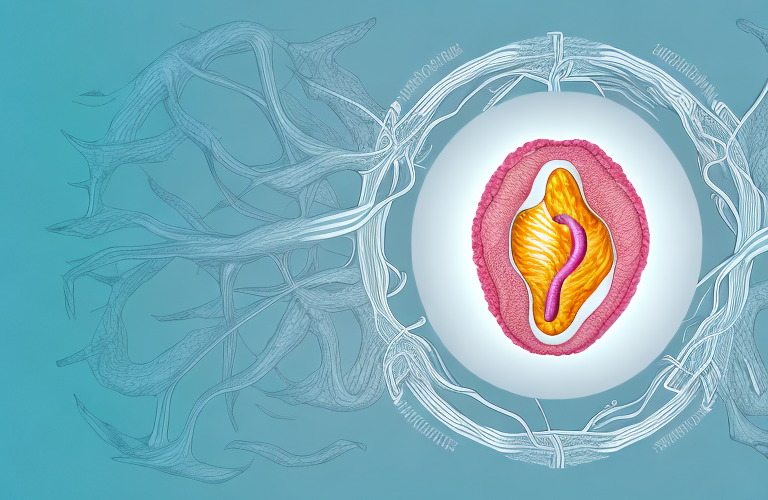
Vaginitis is a common health condition that affects many women at some point in their lives. It is characterized by inflammation of the vagina, which can result in uncomfortable symptoms such as itchiness, burning, and abnormal discharge. In this article, we will discuss the different types of vaginitis, their symptoms, causes, treatment options, as well as provide advice on how to prevent the condition and when to seek medical attention.
What is Vaginitis?
Vaginitis refers to the inflammation of the vaginal lining, which can be caused by a variety of factors such as bacteria, yeast, or parasites. This condition can lead to a range of symptoms, including itching, burning, abnormal discharge, and pain during intercourse. In some cases, vaginitis can also be a sign of an underlying health condition such as a sexually transmitted infection or vaginal atrophy.
It is important to seek medical attention if you experience any symptoms of vaginitis. Your healthcare provider can perform tests to determine the underlying cause of your symptoms and recommend appropriate treatment. Treatment may include antibiotics, antifungal medication, or other medications depending on the cause of the inflammation. Additionally, practicing good hygiene habits and avoiding irritants such as scented products or douching can help prevent vaginitis from occurring.
Types of Vaginitis
There are several different types of vaginitis, each with its own causes and symptoms. The most common types include:
- Bacterial vaginosis
- Yeast infections
- Trichomoniasis
- Atrophic vaginitis
In order to receive the appropriate treatment, it is important to accurately identify the type of vaginitis that is present.
Other less common types of vaginitis include:
- Desquamative inflammatory vaginitis (DIV)
- Non-infectious vaginitis
- Cytolytic vaginosis
- Chemical irritant vaginitis
It is important to note that some types of vaginitis may have similar symptoms, so it is important to consult a healthcare provider for an accurate diagnosis.
Symptoms of Vaginitis
The symptoms of vaginitis can vary depending on the underlying cause. However, some common symptoms include:
- Abnormal vaginal discharge
- Burning or itching in the vaginal area
- Pain during intercourse
- Inflammation of the vaginal area
- Bleeding or spotting between periods
- Foul odor
It is important to note that some women may not experience any symptoms at all.
If you experience any of these symptoms, it is important to see a healthcare provider for an accurate diagnosis and treatment. Vaginitis can be caused by a variety of factors, including bacterial infections, yeast infections, and sexually transmitted infections. Treatment options may include antibiotics, antifungal medication, or other prescription medications. It is also important to practice good hygiene habits, such as wearing breathable cotton underwear and avoiding douching, to prevent vaginitis from occurring.
Causes of Vaginitis
Vaginitis can be caused by a variety of factors, including:
- Bacterial overgrowth
- Fungal infections
- Parasitic infections
- Vaginal atrophy
- Chemical irritants
- Sexually transmitted infections
In order to effectively treat vaginitis, it is important to identify and address the underlying cause.
Bacterial vaginosis is a common cause of vaginitis, and occurs when there is an overgrowth of bacteria in the vagina. This can lead to a fishy odor and discharge.
Another cause of vaginitis is hormonal changes, such as those that occur during pregnancy or menopause. These changes can alter the pH balance of the vagina, leading to inflammation and infection.
Diagnosis of Vaginitis
In order to diagnose vaginitis, a medical professional will take a thorough medical history and perform a physical exam. Additional tests, such as a vaginal swab, may also be necessary to accurately identify the underlying cause of the inflammation. If a sexually transmitted infection is suspected, additional testing may be required.
It is important to note that symptoms of vaginitis can sometimes be similar to those of other vaginal infections, such as yeast infections or bacterial vaginosis. Therefore, it is crucial to seek medical attention if you experience any abnormal vaginal discharge, itching, or discomfort. Early diagnosis and treatment can help prevent complications and improve overall health outcomes.
Treatment Options for Vaginitis
The treatment for vaginitis will depend on the underlying cause. Some common treatment options include:
- Antibiotics
- Antifungal medication
- Antiparasitic medication
- Estrogen therapy (for vaginal atrophy)
In addition to medication, lifestyle changes such as avoiding perfumed products and wearing loose-fitting clothing may also be recommended.
It is important to note that not all cases of vaginitis require medication. In some cases, simply practicing good hygiene habits such as washing the genital area with mild soap and water can help alleviate symptoms. Additionally, incorporating probiotics into your diet or taking probiotic supplements may help maintain a healthy balance of bacteria in the vagina and prevent future cases of vaginitis.
Home Remedies for Vaginitis Relief
Some home remedies may also provide relief for the symptoms of vaginitis. These remedies include:
- Probiotic supplements
- Garlic supplements
- Tea tree oil
- Yogurt supplements
- Boric acid suppositories
It is important to note that these remedies should be used with caution and under the guidance of a healthcare professional.
In addition to these remedies, maintaining good hygiene practices can also help prevent and alleviate symptoms of vaginitis. This includes wearing breathable cotton underwear, avoiding douching and scented products, and wiping from front to back after using the bathroom. It is also important to practice safe sex and to avoid using harsh chemicals or irritants in the genital area.
Preventing Vaginitis: Tips and Advice
There are several steps that can be taken to help prevent vaginitis. These include:
- Avoiding scented products in the vaginal area
- Wearing cotton underwear and loose-fitting clothing
- Practicing safe sex
- Wiping front to back after using the bathroom
- Avoiding douching
By following these guidelines, women can reduce their risk of developing vaginitis.
It is also important to maintain good hygiene practices, such as washing the genital area with mild soap and water daily. Additionally, women should avoid wearing tight clothing or wet bathing suits for extended periods of time, as this can create a moist environment that promotes the growth of bacteria and yeast.
When to See a Doctor for Vaginitis
If a woman experiences vaginal symptoms such as itching, burning, or abnormal discharge, it is important to seek medical attention. This is especially true if symptoms last for more than a few days or if they are accompanied by additional symptoms such as fever or abdominal pain.
It is also important to see a doctor if a woman experiences recurring episodes of vaginitis. Recurrent vaginitis can be a sign of an underlying medical condition that needs to be addressed. Additionally, if a woman is pregnant and experiences vaginal symptoms, she should seek medical attention as soon as possible to ensure the health of both herself and her baby.
When visiting a doctor for vaginitis, it is helpful to keep track of any symptoms and their duration. The doctor may perform a physical exam and take a sample of vaginal discharge to determine the cause of the symptoms. Treatment options may include medication, such as antibiotics or antifungal creams, or lifestyle changes, such as avoiding certain hygiene products or wearing loose-fitting clothing.
The Link between Vaginitis and Sexually Transmitted Infections
Vaginitis can sometimes be a sign of a sexually transmitted infection (STI). It is therefore important to practice safe sex and to receive regular STI testing. If an STI is detected, prompt treatment can help prevent the development of more serious health complications.
There are several types of STIs that can cause vaginitis, including chlamydia, gonorrhea, and trichomoniasis. These infections can be transmitted through sexual contact with an infected partner, and can often be asymptomatic, meaning that a person may not even know they are infected. This is why regular STI testing is so important, even if you are not experiencing any symptoms.
In addition to practicing safe sex and receiving regular STI testing, there are other steps you can take to reduce your risk of developing vaginitis. These include avoiding douching, using unscented or hypoallergenic products in the genital area, and wearing cotton underwear. If you do experience symptoms of vaginitis, such as itching, burning, or abnormal discharge, it is important to see a healthcare provider for an accurate diagnosis and appropriate treatment.
Common Misconceptions about Vaginitis
There are several common misconceptions about vaginitis that can lead to confusion and misunderstanding. Some of these misconceptions include:
- Vaginitis is always caused by a yeast infection.
- Sexual activity always causes vaginitis.
- Vaginitis is a rare condition.
It is important to understand the facts about vaginitis in order to effectively prevent and manage the condition.
One important fact to understand about vaginitis is that it can be caused by a variety of factors, not just yeast infections or sexual activity. Other common causes of vaginitis include bacterial infections, hormonal changes, and certain medications. Additionally, some women may be more prone to developing vaginitis due to factors such as a weakened immune system or the use of certain hygiene products.
How Hormonal Changes Affect the Risk of Developing Vaginitis
Hormonal changes, such as those that occur during menopause, can increase the risk of developing vaginitis. This is because hormonal fluctuations can cause changes in the vaginal environment that make it more susceptible to inflammation and infection. Hormone therapy may be recommended to help manage the symptoms of vaginitis associated with hormonal changes.
It is important to note that hormonal changes are not the only factor that can increase the risk of developing vaginitis. Other factors, such as poor hygiene, certain medications, and underlying medical conditions, can also contribute to the development of vaginitis. It is important to speak with a healthcare provider if you experience symptoms of vaginitis, such as itching, burning, or abnormal discharge, to determine the underlying cause and receive appropriate treatment.
Living with Chronic or Recurrent Vaginal Infections
Chronic or recurrent vaginal infections can be frustrating and difficult to manage. In these cases, it is important to work closely with a healthcare professional to identify and address the underlying cause of the condition. This may involve ongoing treatment with medication and lifestyle changes to help reduce the risk of further infection.
It is also important to maintain good hygiene practices, such as washing the genital area with mild soap and water, wearing clean and breathable underwear, and avoiding the use of scented products that can irritate the vaginal area. Additionally, practicing safe sex by using condoms can help reduce the risk of transmitting or acquiring infections.
Some natural remedies, such as probiotics and tea tree oil, may also be helpful in managing chronic or recurrent vaginal infections. However, it is important to consult with a healthcare professional before trying any new treatments, as they may interact with other medications or have potential side effects.
Natural Supplements and Lifestyle Changes to Support Your Body’s Defense Against Vaginal Infections
In addition to medical treatment, there are several natural supplements and lifestyle changes that can help support the body’s defense against vaginal infections. These may include:
- Probiotic supplements
- Vitamin D supplements
- Reducing stress
- Eating a healthy diet consisting of whole foods
By incorporating these changes into their daily routine, women can help improve their overall health and reduce their risk of developing vaginitis.
In conclusion, vaginitis is a common health condition that can be caused by a variety of factors. It is important to accurately identify the underlying cause of the condition in order to receive appropriate treatment and prevent further complications. By following preventative measures and working closely with a healthcare professional, women can effectively manage the symptoms of vaginitis and improve their overall quality of life.
Another natural supplement that may help support the body’s defense against vaginal infections is garlic. Garlic has been shown to have antimicrobial properties that can help fight off harmful bacteria and fungi. Women can incorporate garlic into their diet by adding it to their meals or taking garlic supplements.
Additionally, practicing good hygiene habits can also help prevent vaginal infections. This includes wearing clean, breathable underwear, avoiding douching, and wiping from front to back after using the bathroom. Women should also avoid using scented products in the genital area, as these can disrupt the natural balance of bacteria and increase the risk of infection.