The hypothalamus is a small but important region in the brain that plays a vital role in regulating many bodily functions. It is responsible for controlling the release of hormones that regulate everything from hunger and thirst to body temperature and sleep. Despite its importance, the hypothalamus is vulnerable to a number of diseases and disorders that can interfere with its normal functioning. In this article, we will explore the various diseases and symptoms associated with the hypothalamus, as well as the treatments available to manage them.
What is the Hypothalamus and What Does it Do?
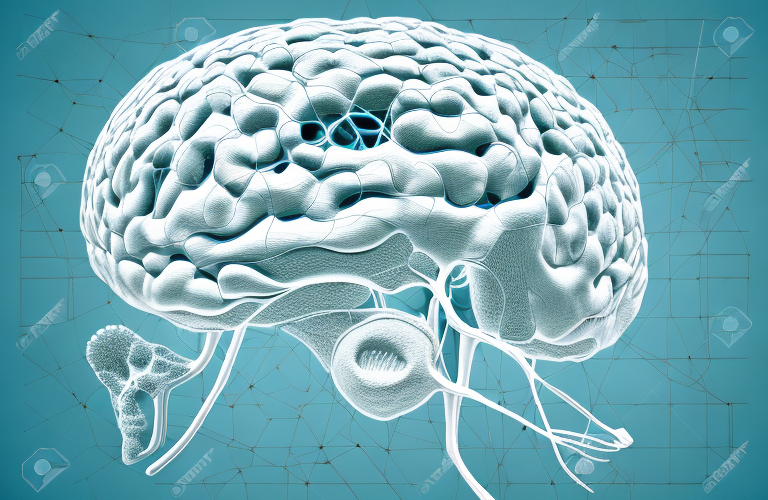
The hypothalamus is a small almond-shaped structure located at the base of the brain. It is a part of the limbic system and sits just above the pituitary gland. The hypothalamus is responsible for many vital functions including regulating the body’s temperature, controlling thirst and hunger, and regulating the body’s sleep-wake cycle. The hypothalamus achieves these functions by releasing a variety of hormones that signal to other parts of the body to either activate or inhibit specific processes.
In addition to its primary functions, the hypothalamus also plays a crucial role in the body’s stress response. When the body experiences stress, the hypothalamus releases a hormone called corticotropin-releasing hormone (CRH), which triggers the release of other stress hormones such as cortisol. This response helps the body to cope with stress and maintain homeostasis. However, chronic stress can lead to dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis, which can have negative effects on physical and mental health.
Understanding Hypothalamic Dysfunction
Hypothalamic dysfunction occurs when the hypothalamus is unable to properly regulate the body’s functions. This can lead to a range of symptoms that can affect a patient’s quality of life and overall health. The causes of hypothalamic dysfunction are varied and can include damage to the hypothalamus as a result of injury or illness, as well as abnormalities in the pituitary gland or other neighboring structures in the brain.
Some of the common symptoms of hypothalamic dysfunction include weight gain or loss, changes in appetite, fatigue, sleep disturbances, and changes in body temperature. Patients may also experience hormonal imbalances, such as irregular menstrual cycles or decreased libido.
Treatment for hypothalamic dysfunction depends on the underlying cause and may include medications, hormone replacement therapy, or surgery. Lifestyle changes, such as maintaining a healthy diet and exercise routine, can also help manage symptoms and improve overall health.
Common Diseases of the Hypothalamus
There are several diseases that can impact the hypothalamus. Some of the most common include hypothalamic hamartoma, hypopituitarism, craniopharyngioma, and idiopathic intracranial hypertension. These diseases can lead to symptoms such as excessive thirst, hunger, and urination, as well as vision problems and hormonal imbalances. Treatment for these conditions may involve medications to regulate hormonal imbalances, surgery to remove tumors, or other interventions such as hormonal replacement therapy.
It is important to note that the hypothalamus plays a crucial role in regulating the body’s temperature, sleep cycles, and stress response. Therefore, damage to the hypothalamus can also lead to disruptions in these functions. Patients with hypothalamic diseases may experience difficulty sleeping, changes in body temperature, and increased stress levels. In some cases, these symptoms can be managed with lifestyle changes such as regular exercise and stress reduction techniques, in addition to medical treatment.
Causes and Risk Factors of Hypothalamic Diseases
The causes of hypothalamic diseases are varied and can include genetic factors, environmental factors, and lifestyle choices. Some risk factors for these diseases may include a family history of hypothalamic disorders, exposure to environmental toxins, or certain medical conditions such as obesity or diabetes.
One of the genetic factors that can contribute to hypothalamic diseases is mutations in genes that regulate the development and function of the hypothalamus. Environmental factors such as exposure to radiation or certain chemicals can also damage the hypothalamus and lead to disease.
Lifestyle choices such as poor diet, lack of exercise, and chronic stress can also increase the risk of developing hypothalamic diseases. These factors can lead to inflammation and oxidative stress in the hypothalamus, which can impair its function and contribute to the development of diseases such as hypothalamic obesity or hypothalamic-pituitary-adrenal (HPA) axis dysfunction.
Symptoms of Hypothalamic Disorders
The symptoms of hypothalamic disorders can vary depending on the specific disease or disorder involved. Common symptoms may include excessive thirst, hunger, and urination, weight gain or loss, fatigue, headaches, and vision problems. Other symptoms may include reduced sexual function, mood changes, and hormonal imbalances.
In addition to the above mentioned symptoms, some hypothalamic disorders may also cause sleep disturbances, such as insomnia or excessive sleepiness. Patients may also experience cognitive changes, such as difficulty with memory or concentration. In rare cases, hypothalamic disorders can lead to seizures or other neurological symptoms. It is important to seek medical attention if you experience any of these symptoms, as early diagnosis and treatment can improve outcomes.
Diagnosis and Treatment of Hypothalamic Disorders
Diagnosis of hypothalamic disorders may involve a variety of tests including blood tests, imaging studies such as MRI or CT scans, and hormone level assessments. Treatment for these disorders may involve medications, hormonal replacement therapy, surgery, or lifestyle changes such as dietary modifications or exercise.
It is important to note that the specific treatment plan for a hypothalamic disorder will depend on the underlying cause of the condition. For example, if the disorder is caused by a tumor, surgery may be necessary to remove the tumor. If the disorder is caused by a hormonal imbalance, hormonal replacement therapy may be prescribed. In some cases, a combination of treatments may be necessary to effectively manage the disorder.
Medications Used to Treat Hypothalamic Dysfunction
There are a variety of medications that may be used to manage hypothalamic dysfunction. These may include medications to regulate hormones, manage symptoms such as headaches or pain, or to prevent or manage complications such as diabetes or hypertension. Your doctor will determine the best course of treatment based on your specific symptoms and medical history.
It is important to note that medication alone may not be enough to manage hypothalamic dysfunction. Lifestyle changes such as a healthy diet, regular exercise, and stress management techniques may also be recommended to help improve symptoms and overall health. Your doctor may also refer you to a specialist, such as an endocrinologist or neurologist, for further evaluation and treatment.
Lifestyle Changes for Managing Hypothalamic Diseases
Lifestyle changes can also be an important part of managing hypothalamic diseases. These may include dietary modifications such as reducing salt intake or avoiding certain foods, exercise, and stress reduction techniques. Working closely with a healthcare provider and following a personalized treatment plan can help to manage symptoms and improve overall health and wellbeing.
In addition to these lifestyle changes, it is also important for individuals with hypothalamic diseases to prioritize getting enough sleep and maintaining a consistent sleep schedule. This can help regulate hormones and improve overall health. It may also be helpful to avoid alcohol and tobacco, as these substances can worsen symptoms and interfere with treatment. By making these lifestyle changes and working closely with a healthcare provider, individuals with hypothalamic diseases can improve their quality of life and manage their condition more effectively.
Coping with the Emotional Impact of Hypothalamic Disorders
Living with a hypothalamic disorder can be challenging, and patients may experience a range of emotional and psychological symptoms as a result. It is important to seek support from family, friends, and healthcare professionals to manage these symptoms and improve overall quality of life. In addition, counseling or support groups may be helpful to manage stress and other emotional symptoms associated with these disorders.
One of the most common emotional symptoms associated with hypothalamic disorders is depression. Patients may feel overwhelmed, hopeless, and experience a loss of interest in activities they once enjoyed. It is important to seek treatment for depression, as it can have a significant impact on overall health and well-being.
Another emotional symptom that may arise is anxiety. Patients may feel anxious about their condition, treatment options, and the impact it may have on their daily life. Learning relaxation techniques, such as deep breathing and meditation, can be helpful in managing anxiety symptoms. Additionally, medication and therapy may be recommended to manage more severe cases of anxiety.
The Connection Between the Hypothalamus and Hormones
The hypothalamus plays a critical role in regulating the body’s hormonal system. It releases hormones that signal to other glands in the body, including the pituitary gland, to produce and release hormones that regulate everything from growth and development to metabolism and stress responses.
Additionally, the hypothalamus is responsible for maintaining homeostasis in the body by regulating body temperature, hunger, thirst, and sleep. It also plays a role in the body’s response to external stimuli, such as light and stress, by releasing hormones that trigger the appropriate response. Without the hypothalamus, the body’s hormonal system would be unable to function properly, leading to a range of health issues.
How Stress Affects the Hypothalamus
Stress can impact the hypothalamus and its ability to regulate the body’s functions. Chronic stress can lead to an overactive hypothalamus, resulting in increased cortisol levels, weight gain, and other negative health consequences. Learning stress reduction techniques, such as meditation or deep breathing, can help to reduce the impact of stress on the hypothalamus and improve overall health and wellbeing.
In addition to the physical effects of stress on the hypothalamus, it can also impact mental health. Chronic stress can lead to anxiety, depression, and other mood disorders. This is because the hypothalamus is responsible for regulating the release of hormones that affect mood, such as serotonin and dopamine. By reducing stress levels, individuals can improve their mental health and reduce the risk of developing mood disorders.
Furthermore, stress can also affect the immune system. The hypothalamus plays a key role in regulating the immune response, and chronic stress can weaken the immune system, making individuals more susceptible to illness and disease. By managing stress levels, individuals can improve their immune function and reduce the risk of developing illnesses such as colds, flu, and infections.
New Research on the Relationship Between the Gut and the Hypothalamus
Recent research has explored the connection between the gut microbiome and hypothalamic function. This research has shown that changes in gut health can impact hypothalamic activity and lead to a range of symptoms and health consequences. Further research in this area may lead to improved treatments for hypothalamic disorders that take into account the role of gut health and microbiome diversity.
One study found that a high-fat diet can alter the gut microbiome and lead to inflammation in the hypothalamus, which can contribute to obesity and metabolic disorders. This highlights the importance of maintaining a healthy gut microbiome through a balanced diet and probiotic supplementation.
Another area of research is exploring the use of fecal microbiota transplantation (FMT) as a potential treatment for hypothalamic disorders. FMT involves transferring fecal matter from a healthy donor to a patient with an imbalanced gut microbiome. While still in the early stages of research, FMT shows promise as a non-invasive and potentially effective treatment option.
Future Directions in Treating Hypothalamic Disorders
As research continues to explore the underlying causes and mechanisms of hypothalamic disorders, new therapies and treatments may emerge. Advances in technologies such as genetic testing and precision medicine may allow for more personalized and targeted treatments for these conditions in the future.
In conclusion, the hypothalamus is a vital brain region that is responsible for many critical bodily functions. Diseases and disorders that impact the hypothalamus can have significant impacts on a patient’s quality of life and overall health. Fortunately, there are many treatments available to manage these conditions, from medications to lifestyle modifications and surgical interventions. By working closely with healthcare providers and following personalized treatment plans, patients with hypothalamic disorders can manage symptoms and improve their overall health and wellbeing.
One area of research that shows promise in treating hypothalamic disorders is the use of stem cells. Stem cells have the ability to differentiate into various types of cells, including those found in the hypothalamus. This could potentially lead to the development of new therapies that can repair or replace damaged hypothalamic cells.
Another area of research is focused on understanding the role of the gut-brain axis in hypothalamic disorders. The gut and the brain are connected through a complex network of nerves and hormones, and disruptions in this communication may contribute to the development of hypothalamic disorders. By better understanding this connection, researchers may be able to develop new treatments that target the gut-brain axis and improve outcomes for patients with these conditions.