Membranoproliferative Glomerulonephritis (MPGN) is a rare but serious kidney disease which causes the glomeruli, the tiny filters in the kidneys responsible for removing wastes and excess liquids from the blood, to become inflamed and damaged. This leads to a build-up of waste products in the body and a decrease in the amount of urine produced. MPGN can affect people of all ages, but it is more commonly diagnosed in adults than children and can lead to kidney failure if left untreated. In this comprehensive guide, we will take a closer look at the symptoms, causes, and treatment options available for MPGN to help you better understand this complex disease.
What is Membranoproliferative Glomerulonephritis (MPGN)?
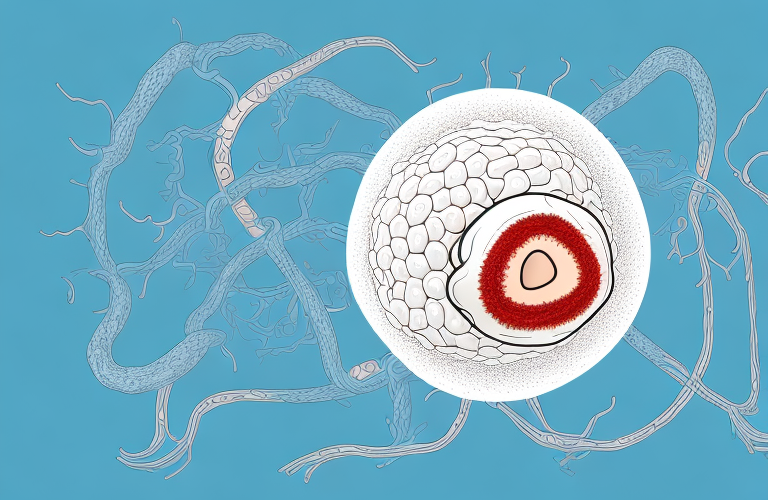
Membranoproliferative Glomerulonephritis (MPGN), also known as mesangiocapillary glomerulonephritis, is a rare type of kidney disease that affects the glomeruli, the tiny filters in the kidneys responsible for removing excess liquids and waste products from the blood. MPGN is characterized by inflammation and thickening of the glomerular capillary walls, which hampers the kidney’s ability to filter the blood efficiently. As a result, waste products and excess fluids accumulate in the body, leading to symptoms such as edema, high blood pressure, and decreased urine output.
MPGN can be caused by a variety of factors, including autoimmune disorders, infections, and genetic mutations. It can also be a complication of other diseases such as hepatitis B and C, lupus, and HIV. Treatment for MPGN typically involves managing symptoms and addressing the underlying cause of the disease. In severe cases, kidney transplant may be necessary.
Types of MPGN: A Comprehensive Overview
There are three types of MPGN, and each has unique characteristics, prognosis, and treatment options. Type 1 MPGN is the most common subtype and is usually idiopathic, meaning there is no known cause. Type 2 MPGN is less common and is associated with a faulty component of the body’s immune system. Type 3 MPGN is the rarest type and is linked to the formation of immune complexes elsewhere in the body, which then deposit in the kidneys and trigger inflammation. Understanding which type of MPGN you have is critical in determining the appropriate treatment and outlook for your condition.
It is important to note that MPGN can also be classified as either primary or secondary. Primary MPGN refers to cases where the disease is the main problem, while secondary MPGN occurs as a result of another underlying condition, such as lupus or hepatitis C. Secondary MPGN can be more challenging to treat, as the underlying condition must also be addressed in order to effectively manage the MPGN. Therefore, it is crucial to work closely with your healthcare provider to determine the cause of your MPGN and develop a comprehensive treatment plan.
Understanding the Pathophysiology of MPGN
The exact pathophysiological mechanisms underlying MPGN are not yet fully understood. It is believed that the disease is triggered when the immune system mistakenly attacks the glomerular capillaries, leading to inflammation and thickening of the walls of these tiny blood vessels. This inflammation leads to dysfunction and eventual destruction of the glomeruli, which impairs kidney function. MPGN can also lead to the formation of scar tissue within the kidneys, which can further impair their ability to function correctly.
Recent studies have suggested that genetic factors may also play a role in the development of MPGN. Certain genetic mutations have been identified in patients with the disease, which may make them more susceptible to developing it. Additionally, environmental factors such as infections and exposure to certain toxins may also contribute to the development of MPGN. Further research is needed to fully understand the complex interplay between genetics and environmental factors in the pathogenesis of MPGN.
What Causes Membranoproliferative Glomerulonephritis?
The exact cause of MPGN is not well understood, and in most cases, the disease is idiopathic, meaning it has no known cause. However, several factors have been associated with the development of MPGN, including viral infections, autoimmune disorders, and certain genetic mutations. Additionally, certain medications and toxins have been found to cause MPGN-like symptoms in some individuals. It’s important to understand the risk factors for developing this disease to help reduce your chances of developing it in the future.
Recent research has suggested that MPGN may also be linked to chronic inflammation in the body. This inflammation can be caused by a variety of factors, including poor diet, lack of exercise, and chronic stress. It’s important to maintain a healthy lifestyle to reduce your risk of developing chronic inflammation and potentially developing MPGN.
While the exact cause of MPGN is still unknown, there are several treatment options available to manage the symptoms and slow the progression of the disease. These treatments may include medications to reduce inflammation, blood pressure medications, and in some cases, dialysis or kidney transplant. It’s important to work closely with your healthcare provider to develop a treatment plan that is tailored to your individual needs.
Symptoms of MPGN: How to Recognize Them
The symptoms of MPGN can vary from person to person and depend on the subtype of MPGN, as well as the severity of the disease. Some of the most common symptoms of MPGN include swelling, particularly around the eyes and ankles, foamy urine, decreased urine output, high blood pressure, and fatigue. It’s important to understand the symptoms of MPGN so that you can seek medical attention promptly, as early diagnosis and treatment may improve your overall prognosis.
Another symptom of MPGN is proteinuria, which is the presence of excess protein in the urine. This can be detected through a urine test and may indicate kidney damage. Additionally, some people with MPGN may experience abdominal pain, nausea, and vomiting, which can be caused by inflammation in the kidneys.
It’s important to note that some people with MPGN may not experience any symptoms at all, especially in the early stages of the disease. This is why regular check-ups with a healthcare provider are important, especially if you have a family history of kidney disease or other risk factors for MPGN.
Diagnostic Tests for Membranoproliferative Glomerulonephritis
To diagnose MPGN, your doctor will likely perform a series of diagnostic tests, including a urinalysis, blood tests, and imaging tests such as an ultrasound or CT scan. Additionally, a kidney biopsy may be required to confirm the diagnosis and determine the subtype of MPGN, as well as to assess the extent of kidney damage. Early detection of MPGN is critical in improving the chances of successful treatment, so it’s essential to undergo regular check-ups and screenings if you’re at risk for this disease.
The urinalysis is a crucial diagnostic test for MPGN, as it can detect the presence of blood and protein in the urine, which are common signs of kidney damage. Blood tests can also help identify abnormalities in kidney function, such as elevated levels of creatinine and urea. Imaging tests, such as an ultrasound or CT scan, can provide detailed images of the kidneys and help identify any structural abnormalities or blockages that may be contributing to the development of MPGN.
In addition to these diagnostic tests, your doctor may also recommend genetic testing to determine if you have any inherited risk factors for MPGN. This can be particularly important for individuals with a family history of kidney disease or those who have previously been diagnosed with other autoimmune disorders. By identifying these risk factors early on, your doctor can develop a personalized treatment plan that addresses your specific needs and helps prevent further kidney damage.
Treatment Options for MPGN: A Comprehensive Guide
The treatment options for MPGN depend on the subtype, severity, and underlying cause of the disease. In general, treatment aims to relieve symptoms, slow the progression of kidney damage, and prevent complications such as kidney failure. Treatment options may include medications such as immunosuppressants or corticosteroids, dialysis, kidney transplant, and lifestyle modifications such as dietary changes and regular exercise. Your doctor will work with you to develop a treatment plan that is tailored to your individual needs, taking into account your overall health, medical history, and other factors that may impact your prognosis.
It is important to note that early detection and treatment of MPGN can greatly improve outcomes and prevent further kidney damage. Regular monitoring of kidney function and blood pressure is recommended for individuals with a history of MPGN or other kidney diseases. Additionally, maintaining a healthy lifestyle, including a balanced diet and regular exercise, can help to manage symptoms and improve overall health.
Medications Used in the Treatment of MPGN
There are several medications used in the treatment of MPGN, such as corticosteroids, immunosuppressants, and angiotensin-converting enzyme (ACE) inhibitors. These medications work by reducing inflammation, slowing the immune system’s response, and regulating blood pressure, respectively. However, these medications can have potential side effects, so it’s important to discuss the benefits and risks of each medication with your healthcare provider before starting treatment.
Corticosteroids are often the first line of treatment for MPGN, as they are effective in reducing inflammation and suppressing the immune system. However, long-term use of corticosteroids can lead to side effects such as weight gain, high blood pressure, and increased risk of infections.
Immunosuppressants, such as cyclophosphamide and azathioprine, are also used in the treatment of MPGN. These medications work by suppressing the immune system, which can help reduce inflammation and slow the progression of the disease. However, they can also increase the risk of infections and may cause other side effects such as nausea, vomiting, and hair loss.
Lifestyle Modifications for Managing MPGN Symptoms
Lifestyle modifications such as dietary changes and regular exercise can help manage the symptoms of MPGN and improve overall health and well-being. People with MPGN may need to limit their intake of certain foods and fluids, such as sodium and protein, to prevent fluid buildup in the body. Additionally, regular exercise can help improve cardiovascular health and maintain a healthy body weight, both of which are important in managing the symptoms of MPGN.
Another important lifestyle modification for managing MPGN symptoms is getting enough rest and managing stress levels. Stress can exacerbate symptoms of MPGN, so it is important to find ways to manage stress, such as practicing relaxation techniques or engaging in activities that bring joy and relaxation.
In addition to lifestyle modifications, people with MPGN may also need medical treatment to manage their symptoms. This may include medications to control blood pressure or reduce inflammation in the kidneys. It is important to work closely with a healthcare provider to develop a comprehensive treatment plan that addresses both lifestyle modifications and medical interventions.
Complications Associated with Membranoproliferative Glomerulonephritis
Complications associated with MPGN can include high blood pressure, anemia, electrolyte imbalances, and kidney failure. If left untreated, MPGN can lead to progressive kidney damage and ultimately result in end-stage renal disease, requiring dialysis or kidney transplant. It’s essential to work with your healthcare provider to monitor and manage these complications and to seek prompt medical attention if you experience any concerning symptoms or changes in your condition.
Another potential complication of MPGN is nephrotic syndrome, which is characterized by high levels of protein in the urine, low levels of protein in the blood, and swelling in various parts of the body. This condition can lead to an increased risk of infections, blood clots, and other health problems.
In some cases, MPGN may be associated with other underlying medical conditions, such as autoimmune disorders or infections. It’s important to work with your healthcare provider to identify and address any underlying causes of MPGN, as this can help to improve treatment outcomes and reduce the risk of complications.
Prevention Strategies for Reducing the Risk of Developing MPGN
Although the exact cause of MPGN is not well understood, there are several steps you can take to reduce your risk of developing this disease. These include maintaining a healthy diet and exercise routine, minimizing exposure to toxic substances, seeking prompt medical attention if you experience any concerning symptoms, and discussing any family history of kidney disease with your healthcare provider. By taking preventative measures, you can help protect your kidney health and reduce your chances of developing MPGN.
Another important prevention strategy for reducing the risk of developing MPGN is to manage any underlying medical conditions that may increase your risk. For example, individuals with autoimmune disorders such as lupus or rheumatoid arthritis may be at a higher risk for developing MPGN. By working closely with your healthcare provider to manage these conditions, you can help reduce your risk of developing MPGN.
In addition, it is important to stay up-to-date on recommended health screenings and check-ups. Regular kidney function tests can help detect any early signs of kidney disease, including MPGN. By catching the disease early, you can work with your healthcare provider to develop a treatment plan and potentially slow the progression of the disease.
Living with MPGN: Tips and Tricks for Coping with the Disease
Coping with the symptoms and lifestyle changes associated with MPGN can be challenging, but there are several tips and tricks you can use to help manage your condition. These may include talking to a healthcare provider, finding a support group, practicing stress-reducing techniques, and taking an active role in your healthcare. Additionally, it’s important to maintain a positive outlook and focus on the things that you can control, such as making healthy lifestyle choices and following your treatment plan.
It’s also important to educate yourself about MPGN and stay up-to-date on the latest research and treatment options. This can help you make informed decisions about your healthcare and feel more empowered in managing your condition. You may also want to consider making lifestyle changes, such as reducing your salt intake and staying hydrated, to help manage your symptoms. Remember, living with MPGN may be challenging, but with the right tools and support, it is possible to lead a fulfilling life.
The Role of Diet in Managing Membranoproliferative Glomerulonephritis
Dietary changes can play a significant role in managing the symptoms of MPGN, particularly in reducing fluid buildup and maintaining a healthy weight. People with MPGN may need to limit their intake of sodium, potassium, and protein and may need to avoid certain foods and beverages, such as alcohol and caffeine. Additionally, it’s important to stay hydrated and maintain a balanced diet to help manage your condition effectively.
In conclusion, Membranoproliferative Glomerulonephritis (MPGN) is a rare but serious kidney disease that affects people of all ages. Understanding the symptoms, causes, and treatment options available for MPGN is critical in improving diagnosis, treatment, and prognosis for this complex disease. By taking preventative measures, making lifestyle modifications, and following an individualized treatment plan, people with MPGN can manage their symptoms effectively and improve their overall health and well-being.
Another important aspect of managing MPGN through diet is to limit the intake of phosphorus. High levels of phosphorus in the blood can lead to bone disease and other complications. Foods that are high in phosphorus include dairy products, nuts, and whole grains. It’s important to work with a registered dietitian to develop a meal plan that is low in phosphorus and meets your individual nutritional needs.
Furthermore, people with MPGN may benefit from incorporating anti-inflammatory foods into their diet. Chronic inflammation is a common feature of MPGN and can contribute to kidney damage. Foods that have anti-inflammatory properties include fatty fish, leafy greens, berries, and nuts. By including these foods in your diet, you may be able to reduce inflammation and improve your overall health.