Peptic stricture is a medical condition that affects the digestive system. It is characterized by the narrowing of the esophagus due to scar tissue formation or inflammation, leading to difficulty swallowing and other discomfort. This article discusses everything you need to know about peptic stricture, including its causes, symptoms, diagnosis, treatment, and prevention.
What is Peptic Stricture?
Peptic stricture is a condition that occurs when the esophagus, the muscular tube that connects the throat to the stomach, becomes narrow or blocked. This narrowing can make it difficult for food and liquids to pass through the esophagus and can cause a range of symptoms, including difficulty swallowing, chest pain, and heartburn.
Peptic stricture is most commonly caused by long-term acid reflux, which can damage the lining of the esophagus and lead to scarring. Other causes may include frequent vomiting, radiation therapy, and certain medications. If left untreated, peptic stricture can lead to complications such as malnutrition and weight loss. Treatment options may include medication to reduce acid reflux, stretching or dilation of the esophagus, or surgery in severe cases.
Understanding the Digestive System
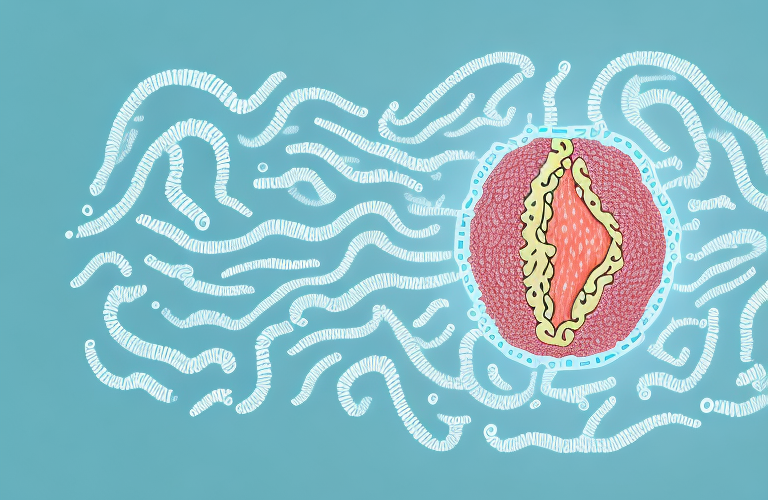
To understand how peptic stricture occurs, it helps to know a bit about the digestive system. The digestive system is a complex network of organs and tissues that work together to break down food, absorb nutrients, and eliminate waste. The process begins in the mouth, where saliva helps to break down food and enzymes begin to digest carbohydrates.
The food then travels down the esophagus and into the stomach, where gastric acid and other enzymes continue the digestion process. The stomach also contracts and churns the food to further break it down into a liquid consistency before passing it into the small intestine. The small intestine is where most of the nutrients from the food are absorbed into the bloodstream, whereas the large intestine absorbs water and eliminates waste products from the body.
It is important to note that the digestive system is not just responsible for breaking down food, but also plays a crucial role in the body’s immune system. The digestive tract is lined with immune cells that help to protect the body from harmful bacteria and viruses that may be present in the food we eat. These immune cells work together with the gut microbiome, a collection of microorganisms that live in the digestive tract, to maintain a healthy balance and prevent infections.
Additionally, certain lifestyle factors can have a significant impact on the digestive system. For example, a diet high in processed foods and low in fiber can lead to constipation and other digestive issues. Stress and lack of sleep can also disrupt the digestive system, leading to symptoms such as bloating, diarrhea, and abdominal pain. Therefore, it is important to maintain a healthy lifestyle and diet to support optimal digestive health.
How Does Peptic Stricture Occur?
Peptic stricture occurs when the lining of the esophagus becomes inflamed or damaged, leading to the formation of scar tissue. This scar tissue can make the esophagus narrower and more rigid, making it harder for food and liquids to pass through.
The condition is commonly associated with gastroesophageal reflux disease (GERD), a digestive disorder characterized by the backward flow of stomach acid into the esophagus. This can irritate and damage the lining of the esophagus, leading to inflammation and scar tissue formation. Other causes of peptic stricture include long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs) and rare conditions like eosinophilic esophagitis or achalasia.
Peptic stricture can cause a range of symptoms, including difficulty swallowing, chest pain, and heartburn. In severe cases, it can lead to weight loss and malnutrition due to the inability to eat and drink properly.
Treatment for peptic stricture typically involves addressing the underlying cause, such as managing GERD or discontinuing NSAID use. In some cases, surgery may be necessary to widen the esophagus and improve swallowing function. Lifestyle changes, such as avoiding trigger foods and eating smaller, more frequent meals, can also help manage symptoms and prevent further damage to the esophagus.
Common Symptoms of Peptic Stricture
The symptoms of peptic stricture can vary from person to person, and may develop gradually or suddenly. Common symptoms include difficulty swallowing (dysphagia), chest pain, regurgitation of food or liquids, heartburn, and unintended weight loss. In some cases, people may also experience coughing, hoarseness, or wheezing.
Peptic stricture is a condition that occurs when the lining of the esophagus becomes damaged due to long-term acid reflux. This can cause scar tissue to form, which can narrow the esophagus and make it difficult to swallow. If left untreated, peptic stricture can lead to more serious complications, such as esophageal ulcers or even esophageal cancer.
There are several factors that can increase your risk of developing peptic stricture, including obesity, smoking, and a diet high in acidic or spicy foods. Treatment for peptic stricture typically involves medications to reduce acid reflux, as well as lifestyle changes such as weight loss and avoiding trigger foods. In severe cases, surgery may be necessary to widen the esophagus and improve swallowing function.
When to Seek Medical Attention for Peptic Stricture
If you experience any of the above symptoms, you should seek medical attention right away. Peptic stricture can be a serious condition that can lead to complications like bleeding, aspiration (inhaling food or stomach acid), and esophageal cancer if left untreated.
Your doctor will likely perform a number of tests to diagnose peptic stricture, including an upper endoscopy, barium swallow test, or esophageal manometry. Treatment options for peptic stricture depend on the severity of the condition and the underlying cause.
In addition to seeking medical attention, there are also some lifestyle changes that can help manage peptic stricture. These include avoiding foods that trigger acid reflux, eating smaller meals more frequently throughout the day, and avoiding lying down for at least two hours after eating.
If your peptic stricture is caused by an underlying condition like GERD or H. pylori infection, treating that condition may also help alleviate symptoms and prevent further damage to the esophagus.
Diagnosis of Peptic Stricture: Tests and Procedures
To diagnose peptic stricture, your doctor may recommend one or more of the following tests and procedures:
- Upper endoscopy: This procedure involves inserting a thin, flexible tube with a camera at the end into the esophagus to visualize the lining and look for any abnormalities.
- Barium swallow test: This test involves swallowing a liquid containing barium, a contrast material that allows the esophagus to show up more clearly on X-rays. The X-rays can help identify any narrowing or blockage in the esophagus.
- Esophageal manometry: This procedure measures the pressure and coordination of the muscles in the esophagus during swallowing. It can help identify any problems with the muscular contractions that may be contributing to the stricture.
In addition to these tests, your doctor may also recommend:
- Biopsy: During an upper endoscopy, your doctor may take a small tissue sample (biopsy) from the lining of the esophagus to check for inflammation, infection, or abnormal cells.
- pH monitoring: This test involves inserting a small tube through the nose and into the esophagus to measure the amount of acid reflux. It can help determine if acid reflux is contributing to the development of the peptic stricture.
It is important to follow your doctor’s recommendations for testing and diagnosis to ensure proper treatment and management of peptic stricture.
Treatment Options for Peptic Stricture: A Comprehensive Guide
Treatment options for peptic stricture depend on the underlying cause and the severity of the condition. Common treatments include:
- Medications: Your doctor may recommend one or more medications to reduce inflammation, relieve symptoms, and prevent complications. These may include proton pump inhibitors, H2 blockers, antacids, or corticosteroids, depending on the underlying cause and severity of the stricture.
- Dilation: This procedure involves stretching the esophagus using a balloon or other device to widen the narrow section of the esophagus. This can help alleviate symptoms and improve swallowing function, but it may need to be repeated periodically to maintain the results.
- Surgery: In some cases, surgery may be necessary to repair or remove damaged portions of the esophagus and relieve symptoms of peptic stricture.
Aside from the common treatments mentioned above, there are also alternative therapies that may help manage peptic stricture. These include:
- Acupuncture: This traditional Chinese medicine practice involves inserting thin needles into specific points on the body to stimulate healing and relieve pain. Some studies suggest that acupuncture may help reduce inflammation and improve symptoms of peptic stricture.
- Herbal remedies: Certain herbs, such as licorice root, slippery elm, and marshmallow root, may help soothe the esophagus and reduce inflammation. However, it is important to consult with a healthcare provider before using any herbal remedies, as they may interact with other medications or have side effects.
In addition to these treatments, lifestyle modifications can also play a role in managing peptic stricture. These may include:
- Dietary changes: Avoiding trigger foods, such as spicy or acidic foods, and eating smaller, more frequent meals may help reduce symptoms of peptic stricture.
- Weight management: Maintaining a healthy weight can help reduce pressure on the esophagus and improve symptoms.
- Smoking cessation: Quitting smoking can help reduce inflammation and improve overall health, which may in turn improve symptoms of peptic stricture.
Medications for Peptic Stricture: Pros and Cons
Medications are often used to treat peptic stricture, and while they can be effective, they also have some potential drawbacks. For example, proton pump inhibitors can increase the risk of certain infections, such as pneumonia and Clostridium difficile. Long-term NSAID use can also increase the risk of gastrointestinal bleeding and ulcers. Your doctor will weigh the benefits and risks of each medication and help you make an informed decision about your treatment options.
Another potential drawback of medications for peptic stricture is that they may not provide long-term relief. In some cases, the stricture may return once the medication is discontinued. Additionally, some patients may experience side effects from the medication, such as headaches, nausea, or diarrhea.
However, medications can also be a convenient and non-invasive treatment option for peptic stricture. They can be taken orally and do not require any surgical procedures. They may also be less expensive than other treatment options, such as endoscopic dilation or surgery.
Surgical Treatments for Peptic Stricture: Types, Risks, and Benefits
Surgery is typically reserved for cases where other treatments have been unsuccessful or the stricture is severe. There are several types of surgical procedures that can be used, including:
- Nissen fundoplication: This surgery involves wrapping the upper part of the stomach around the lower esophageal sphincter to reinforce it and prevent reflux.
- Heller myotomy: This procedure involves cutting the lower esophageal sphincter to prevent it from contracting too much and interfering with swallowing.
- Esophageal resection: This surgery involves removing part or all of the esophagus and reconstructing it using a portion of the stomach or intestine.
Like any surgery, these procedures carry risks and potential complications, including bleeding, infection, and anesthesia-related complications. Your doctor will discuss the benefits and risks of each procedure with you and help you make an informed decision about the best treatment options for your situation.
It is important to note that surgical treatments for peptic stricture are not always a permanent solution. In some cases, the stricture may recur or new strictures may develop. Additionally, recovery from surgery can be lengthy and may require significant lifestyle changes, such as a restricted diet or limited physical activity. It is important to discuss all aspects of surgical treatment with your doctor and carefully weigh the potential benefits and risks before making a decision.
Lifestyle Changes to Manage Peptic Stricture Symptoms
In addition to medical and surgical treatments, there are several lifestyle changes you can make to help manage your peptic stricture symptoms, including:
- Eating smaller, more frequent meals: This can help reduce pressure on the esophagus and make swallowing easier.
- Avoiding trigger foods and beverages: Certain foods and drinks, such as fatty foods, citrus, and alcohol, can aggravate symptoms of acid reflux and peptic stricture.
- Not lying down after eating: This can increase the chances of acid reflux and worsen symptoms of peptic stricture.
Aside from the aforementioned lifestyle changes, there are other ways to manage peptic stricture symptoms. One of which is by maintaining a healthy weight. Being overweight or obese can increase the pressure on your stomach, which can lead to acid reflux and worsen your symptoms. Regular exercise and a balanced diet can help you achieve and maintain a healthy weight.
Another way to manage peptic stricture symptoms is by avoiding smoking and secondhand smoke. Smoking can weaken the lower esophageal sphincter, which is responsible for preventing stomach acid from flowing back into the esophagus. This can lead to acid reflux and worsen your symptoms. Quitting smoking or avoiding secondhand smoke can help improve your condition.
Prevention of Peptic Stricture: Tips and Strategies
While there is no surefire way to prevent peptic stricture, there are several strategies you can use to reduce your risk of developing the condition, including:
- Managing acid reflux: Acid reflux is a common cause of peptic stricture, so managing the condition can help reduce your risk of developing the stricture.
- Avoiding NSAIDs: Long-term use of NSAIDs can increase the risk of gastrointestinal bleeding and ulcers, which can lead to peptic stricture.
- Quitting smoking: Smoking can irritate the lining of the esophagus and increase the risk of inflammation and scarring.
Aside from the aforementioned strategies, there are other ways to prevent peptic stricture. One of which is to maintain a healthy diet. Eating a balanced diet that is rich in fiber, fruits, and vegetables can help prevent acid reflux and other digestive problems that can lead to peptic stricture.
Another way to prevent peptic stricture is to manage stress. Stress can trigger acid reflux and other digestive problems, which can lead to peptic stricture. Practicing relaxation techniques such as yoga, meditation, and deep breathing can help reduce stress and prevent the condition.
Managing Complications of Peptic Stricture: What You Need to Know
If left untreated, peptic stricture can lead to a range of complications, including bleeding, aspiration, and esophageal cancer. If you experience any of the symptoms of peptic stricture, you should seek medical attention right away to prevent complications from developing.
One of the most common complications of peptic stricture is difficulty swallowing, also known as dysphagia. This can lead to malnutrition and dehydration if left untreated. In severe cases, a feeding tube may be necessary to ensure adequate nutrition.
Another potential complication of peptic stricture is the development of Barrett’s esophagus, a condition in which the cells lining the esophagus change and become more similar to those found in the intestine. This can increase the risk of developing esophageal cancer. Regular monitoring and treatment of peptic stricture can help prevent the development of Barrett’s esophagus and reduce the risk of cancer.
The Role of Diet in Managing Peptic Stricture
Diet can play a role in managing peptic stricture symptoms, and certain foods and beverages can exacerbate acid reflux and make symptoms worse. Common trigger foods include spicy foods, coffee, citrus, and fatty foods. Your doctor may recommend a specific diet or food plan to help manage your symptoms and reduce your risk of complications.
In addition to avoiding trigger foods, it is important to eat smaller, more frequent meals throughout the day to help reduce the amount of acid in your stomach. Eating slowly and chewing your food thoroughly can also help prevent symptoms. It is also recommended to avoid eating within 2-3 hours of bedtime to allow your stomach to empty before lying down. Your doctor may also recommend certain supplements, such as probiotics or digestive enzymes, to help improve digestion and reduce inflammation in the digestive tract.
Support Groups and Resources for People with Peptic Stricture
Living with peptic stricture can be challenging, but there are resources available to help. Support groups and online forums can provide a space for people with peptic stricture to connect, share information, and find emotional support. Your doctor may also be able to provide you with information on local resources and support groups.
Peptic stricture is a serious medical condition that can cause a range of symptoms and complications. If you experience any of the symptoms of peptic stricture, it is important to seek medical attention right away to prevent further damage to your esophagus and reduce your risk of complications. With the right treatment plan and lifestyle changes, however, most people with peptic stricture can successfully manage their symptoms and lead a healthy, fulfilling life.
It is important to note that peptic stricture can be caused by long-term acid reflux, which can be managed through lifestyle changes such as avoiding trigger foods, losing weight, and elevating the head of your bed while sleeping. Your doctor may also prescribe medications to reduce acid production in your stomach and promote healing of your esophagus. In severe cases, surgery may be necessary to widen the narrowed area of your esophagus. It is important to work closely with your healthcare team to develop a treatment plan that is right for you and to attend regular follow-up appointments to monitor your condition.