Vaginal cancer is a rare type of cancer that affects the tissues of the vagina. It can develop at any age, but it is most commonly found in women who are over the age of 60. In this article, we will provide a comprehensive overview of vaginal cancer, including its symptoms, causes, treatment options, and more.
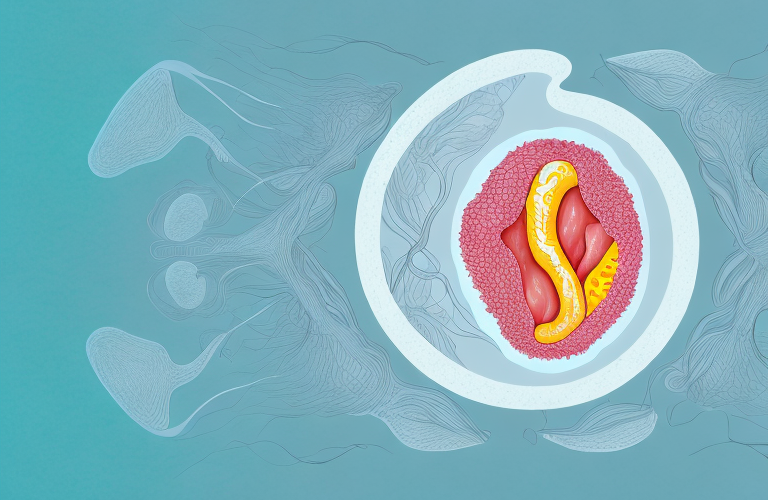
Understanding Vaginal Cancer: An Overview
Vaginal cancer is a type of cancer that develops in the tissues of the vagina, which is the muscular tube that connects the cervix (the lower part of the uterus) to the external genitals. There are several types of vaginal cancer, including squamous cell carcinoma, adenocarcinoma, and sarcoma.
The exact cause of vaginal cancer is not known, but certain factors can increase the risk of developing the disease. These include a history of cervical cancer, exposure to diethylstilbestrol (DES) in utero, smoking, and a weak immune system.
Early detection of vaginal cancer is crucial for successful treatment. Symptoms of vaginal cancer may include abnormal vaginal bleeding, pain during intercourse, and a lump or mass in the vagina. If you experience any of these symptoms, it is important to see a healthcare provider for evaluation.
Treatment for vaginal cancer may include surgery, radiation therapy, chemotherapy, or a combination of these treatments. The type of treatment recommended will depend on the stage and type of cancer, as well as the patient’s overall health and preferences.
What are the Causes of Vaginal Cancer?
The exact cause of vaginal cancer is not known, but there are several risk factors that can increase a woman’s likelihood of developing the disease. These include:
- A history of cervical or vulvar cancer
- Exposure to diethylstilbestrol (DES) in utero
- Smoking
- A weak immune system
While the exact cause of vaginal cancer is unknown, research has shown that certain strains of the human papillomavirus (HPV) can increase a woman’s risk of developing the disease. HPV is a common sexually transmitted infection that can cause genital warts and abnormal cell growth in the cervix, vagina, and anus.
Other risk factors for vaginal cancer include age, with the majority of cases occurring in women over the age of 50, and a family history of the disease. Additionally, women who have had a hysterectomy, particularly one that involved the removal of the cervix, may be at an increased risk for vaginal cancer.
Symptoms of Vaginal Cancer: What to Look Out For
Some of the most common symptoms of vaginal cancer include:
- Abnormal vaginal bleeding (e.g., bleeding after intercourse, bleeding between periods, or postmenopausal bleeding)
- Pain during sexual intercourse
- Pain or discomfort in the pelvic area
- A lump or mass in the vagina
- Changes in vaginal discharge (e.g., an increase in amount or a foul smell)
It is important to note that these symptoms can also be caused by other, less serious conditions. Nevertheless, if you experience any of these symptoms, you should see a healthcare provider right away for an evaluation.
There are several risk factors that can increase a woman’s chances of developing vaginal cancer. These include:
- Being over the age of 50
- Having a history of abnormal cells in the cervix or vagina
- Having a weakened immune system
- Having a history of smoking
- Having a history of human papillomavirus (HPV) infection
It is important for women to be aware of these risk factors and to discuss them with their healthcare provider.
Fortunately, vaginal cancer is rare and can often be treated successfully if caught early. Treatment options may include surgery, radiation therapy, and chemotherapy. Your healthcare provider can help determine the best course of treatment for you based on the stage and location of the cancer.
Different Stages of Vaginal Cancer and Their Treatment Options
The treatment for vaginal cancer depends on the stage of the disease, which is determined by the size of the tumor and whether it has spread to other parts of the body. There are four stages of vaginal cancer, each with its own treatment options:
Stage 0
In this stage, the cancer is only located in the lining of the vagina and has not spread to other parts of the body. Treatment for stage 0 vaginal cancer typically involves surgery to remove the cancerous tissue.
Stage I
In this stage, the cancer has spread beyond the lining of the vagina but has not yet reached the lymph nodes or other organs. Treatment for stage I vaginal cancer typically involves surgery and radiation therapy.
Stage II
In this stage, the cancer has spread to the connective tissue surrounding the vagina but has not yet reached the lymph nodes or other organs. Treatment for stage II vaginal cancer typically involves surgery, radiation therapy, and sometimes chemotherapy.
Stage III and IV
In these stages, the cancer has spread to the lymph nodes or other organs in the body. Treatment for stage III and IV vaginal cancer typically involves a combination of surgery, radiation therapy, and chemotherapy.
It is important to note that early detection of vaginal cancer can greatly increase the chances of successful treatment. Regular gynecological exams and Pap tests can help detect any abnormalities in the vaginal area.
Additionally, some risk factors for vaginal cancer include smoking, having a weakened immune system, and being exposed to the drug diethylstilbestrol (DES) while in the womb. It is important to discuss any potential risk factors with your healthcare provider.
Diagnosing Vaginal Cancer: Tests and Procedures
If a healthcare provider suspects that you may have vaginal cancer, he or she may recommend several tests and procedures to make a definitive diagnosis. These may include:
- Physical exam and pelvic exam.
- Colposcopy.
- Biopsy.
- Imaging tests, such as CT scan, MRI, or PET scan.
It is important to note that these tests and procedures are not always conclusive, and further testing may be necessary. In some cases, a healthcare provider may recommend genetic testing to determine if there is a hereditary component to the cancer. Additionally, if the cancer has spread beyond the vaginal area, a biopsy of other affected areas may be necessary to determine the extent of the cancer and the best course of treatment.
Surgery as a Primary Treatment for Vaginal Cancer
Surgery is often the primary treatment for vaginal cancer, particularly in the early stages of the disease. The type of surgery will depend on the location and extent of the cancer. Some common surgical procedures used to treat vaginal cancer include:
- Laser surgery.
- Wide local excision.
- Vaginectomy.
- Hysterectomy.
It is important to note that surgery may not be the only treatment option for vaginal cancer. In some cases, radiation therapy or chemotherapy may be used in combination with surgery to increase the effectiveness of treatment. Additionally, the decision to undergo surgery as a primary treatment for vaginal cancer should be made in consultation with a healthcare provider who can provide personalized recommendations based on the individual’s specific case and medical history.
Radiation Therapy for Vaginal Cancer: How it Works
Radiation therapy is another common treatment for vaginal cancer. It involves the use of high-energy radiation to kill cancer cells. There are two main types of radiation therapy: external beam radiation therapy and brachytherapy.
External beam radiation therapy involves the use of a machine outside the body to deliver radiation to the affected area. Brachytherapy involves the insertion of a small, radioactive source into the vagina to deliver radiation directly to the tumor.
External beam radiation therapy is typically given in daily doses over several weeks. During treatment, the patient lies on a table while the machine delivers radiation to the affected area. The radiation is carefully targeted to avoid damaging healthy tissue surrounding the tumor.
Brachytherapy is often used in combination with external beam radiation therapy. It can be given as a one-time treatment or in multiple sessions. The radioactive source is inserted into the vagina and left in place for a specific amount of time before being removed. This allows for a high dose of radiation to be delivered directly to the tumor while minimizing exposure to healthy tissue.
Chemotherapy for Vaginal Cancer: What You Need to Know
Chemotherapy is a treatment that uses drugs to kill cancer cells. It is often used in combination with other treatments, such as surgery and radiation therapy. Chemotherapy drugs may be given orally or administered intravenously.
Some common chemotherapy drugs used to treat vaginal cancer include cisplatin, paclitaxel, and 5-fluorouracil.
Chemotherapy can have side effects, such as nausea, vomiting, hair loss, and fatigue. These side effects can vary depending on the type and dosage of chemotherapy drugs used. Your healthcare team will work with you to manage any side effects you may experience.
It is important to follow your healthcare team’s instructions for chemotherapy treatment, including attending all scheduled appointments and taking medications as prescribed. Chemotherapy can be a challenging treatment, but it can also be an effective way to fight vaginal cancer and improve your overall health and well-being.
Alternative Treatments for Vaginal Cancer
While traditional treatments such as surgery, radiation, and chemotherapy are often recommended for vaginal cancer, some people may choose to supplement these treatments with alternative therapies, such as acupuncture, massage, or herbal remedies.
It is important to discuss any alternative treatment options with your healthcare provider to ensure that they are safe and will not interfere with your traditional treatment plan.
Some alternative therapies that have shown promise in managing symptoms and improving quality of life for vaginal cancer patients include meditation, yoga, and aromatherapy. These practices can help reduce stress and anxiety, improve sleep, and promote relaxation.
Coping with the Emotional Impact of a Vaginal Cancer Diagnosis
A diagnosis of vaginal cancer can be overwhelming and stressful. It is important to seek emotional support from family and friends, as well as professional counselors or support groups. You may also find it helpful to explore coping strategies, such as mindfulness meditation or yoga.
It is also important to take care of your physical health during this time. Eating a balanced diet and engaging in regular exercise can help improve your overall well-being and reduce stress. Additionally, it is important to follow your doctor’s recommended treatment plan and attend all scheduled appointments. Remember to be kind to yourself and take things one day at a time.
Tips for Preventing Vaginal Cancer
While there is no sure way to prevent vaginal cancer, there are several steps you can take to reduce your risk:
- Get regular Pap tests and gynecological exams.
- Avoid smoking.
- Use condoms during sex to reduce your risk of sexually transmitted infections.
- Eat a healthy diet and maintain a healthy weight.
- Discuss the risks and benefits of hormone replacement therapy with your healthcare provider.
In addition to the above steps, there are other lifestyle changes you can make to reduce your risk of developing vaginal cancer. One of the most important is to limit your exposure to human papillomavirus (HPV), which is a major risk factor for this type of cancer. You can do this by getting vaccinated against HPV and practicing safe sex.
Another way to reduce your risk of vaginal cancer is to avoid using douches or other feminine hygiene products that can disrupt the natural balance of bacteria in your vagina. This can increase your risk of infection and inflammation, which can in turn increase your risk of cancer.
Living with and Beyond Vaginal Cancer: Life After Treatment
After completing treatment for vaginal cancer, it is important to continue to follow up with your healthcare provider with regular exams to monitor for any signs of recurrence. You may also benefit from working with a cancer rehabilitation specialist to address any physical or emotional challenges you may be experiencing.
In addition to medical follow-up, it is important to take care of your overall health and well-being. This may include making healthy lifestyle choices such as eating a balanced diet, getting regular exercise, and managing stress. You may also find it helpful to connect with other cancer survivors or join a support group to share your experiences and receive emotional support.
It is also important to be aware of potential long-term side effects of treatment, such as vaginal dryness or scarring. Your healthcare provider can provide guidance on managing these symptoms and improving your quality of life. Remember to prioritize self-care and seek support when needed as you navigate life after vaginal cancer treatment.
Understanding the Prognosis of Vaginal Cancer
The prognosis for vaginal cancer depends on a variety of factors, including the stage of the disease and the individual’s overall health. With prompt diagnosis and treatment, however, many people with vaginal cancer are able to achieve remission and live full, healthy lives.
In conclusion, vaginal cancer is a rare but serious condition that requires prompt diagnosis and treatment. By being aware of the symptoms, taking steps to reduce your risk, and seeking the care of qualified healthcare providers, you can increase your chances of achieving a positive outcome.
It is important to note that regular gynecological exams and Pap tests can help detect vaginal cancer in its early stages, when it is most treatable. Additionally, quitting smoking and practicing safe sex can also reduce your risk of developing vaginal cancer. If you experience any symptoms such as abnormal vaginal bleeding or discharge, pain during sex, or pelvic pain, it is important to seek medical attention right away.